*Please note that this post contains clearly identified affiliate links. If you click on these link and choose to make a purchase, I may receive a commission (at no cost to you). As an Amazon Associate I earn from qualifying purchases.
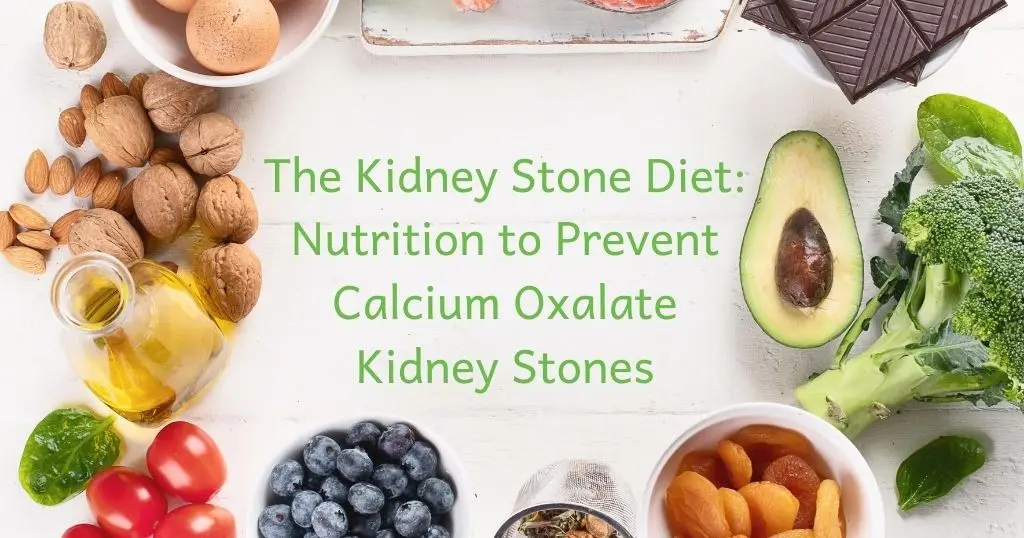
Did you know that a healthy diet can directly reduce your risk for kidney stones? Nutrition is a critical piece of kidney stone prevention that is often overlooked. In fact, a study found that 75% of urology patients didn’t know how nutrition effects kidney stones!(1) Healthy eating for kidney stones can seen overwhelming. There is a ton of information online that is inaccurate and not based on quality science. This has led to conflicting information and confusion about what a healthy kidney stone diet actually is.
Keep reading to learn about what the evidenced-based kidney stone diet is and what you can do to prevent calcium oxalate kidney stones!
Table of Contents
Prevalence of Kidney Stones
Kidney stones are surprisingly common, and have become more common in recent years.(2) The prevalence of kidney stones has more than tripled in the past 40 years. About 1 in 10 people in the United States will have a symptomatic kidney stone at some point in life. However, there are likely many more people who have had kidney stones without symptoms. Kidney stones are more common in men (10.9% compared to 9.4% in women). However, most of the increase in kidney stone prevalence can be attributed to higher numbers of women forming kidney stones.(2)
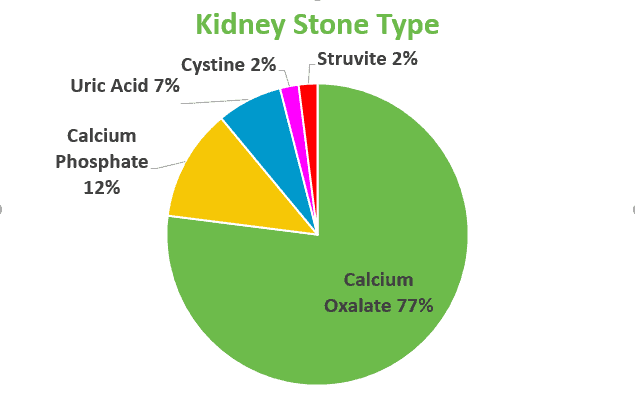
Calcium oxalate is by far the most common type of kidney stone. Around 80% of kidney stones are made of calcium & oxalate. Calcium phosphate stones are the second most common, comprising around 10% of kidney stones. Kidney stones can also be formed from uric acid, struvite and cystine. This article focuses on calcium oxalate kidney stones, as they are by far the most common and usually most diet-related. The other stone types do have some dietary considerations, but a healthy diet is different than the information covered in this article.
What Makes a Kidney Stone?
Supersaturation
Ultimately, calcium oxalate kidney stones form from high concentrations of calcium and oxalate in urine. The more calcium and oxalate in, the higher the risk that these two molecules will bind and form a kidney stone. The amount of these two molecules in the urine, combined with your urine volume, determines your calcium oxalate urine supersaturation. Your calcium oxalate supersaturation should be included in the results of 24-hour urine tests.
Therefore, the kidney stone diet aims to reduce calcium and oxalate in the urine as well as increase your urine volume to reduce supersaturation.
Urine pH
Urine pH also plays a role in kidney stone formation. Urine that is too acidic (or, the pH is too low) increases the risk of calcium oxalate kidney stones. Calcium and oxalate are more likely to bind in acidic environments. So, the kidney stone diet aims to increase urine pH to reduce the risk that calcium and oxalate will bind.
High Risk Groups
The majority of calcium oxalate kidney stones are formed due to “idiopathic hypercalcuria”. Or, high calcium in the urine from unknown causes. There is likely a genetic component here, however, genetics likely does not explain the whole story. Unhealthy diet likely plays a large role in high calcium levels in urine for many people.(3)
In addition, some medical conditions put people at higher risk of kidney stones: (3)
- Gout
- Hyperparathyroidism
- Renal Tubule Acidosis (RTA)
- Cystinuria
- Dent’s Disease
- Primary Hyperoxaluria (PH1)
- Sarcoidosis
- Medullary Sponge Disease (MSK)
- Eating Disorders (especially those who misuse laxatives or who induce vomiting)
Also, some groups of people form kidney stones more often:(3)(4)(5)
- Males
- Caucasians
- Bariatric surgery patients
- People who do not eat a healthy diet
- People who are above their healthy body weight
Kidney Stone Diet Goals
The goals of the kidney stone diet really boil down to 4 distinct outcomes. Each of the kidney stone diet components works to get us to at least one of these goals.
- Increase urine volume (drink fluid)
- Increase urine pH to a healthy range (limit protein, eat lots of fruits & vegetables)
- Reduce urine calcium (limit salt, sugar & protein)
- Reduce urine oxalate (eat calcium, limit oxalate and protein)
A healthy kidney stone diet is different for every single person. A 24-hour urine test is critical to know what pieces of nutrition for calcium oxalate stones will matter for you!
The 7 Pillars of the Kidney Stone Diet
Here are the 7 most important components of eating for kidney stone prevention. I have created a character for us, who I have lovingly named “Mr. McStoney”, to help us understand each of these components.
1. Drink Lots of Fluid
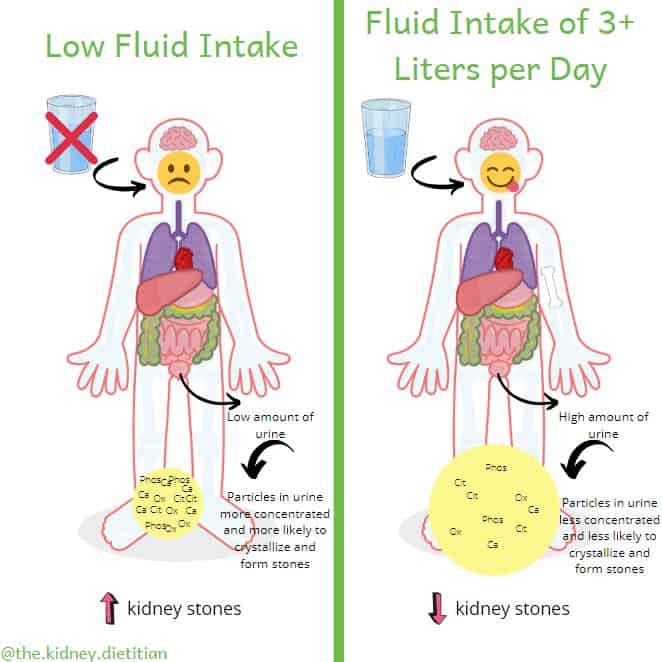
In order to meet our kidney stone diet goal #1 of increasing urine volume, we need to drink more! Nearly all of the fluid you drink (or eat, from foods that contain a lot of water) will be made into urine. Some fluid is lost from things like breathing, feces and sweat.
The more urine you make, the less concentrated calcium and oxalate molecules will be, making it less likely a kidney stone with form.
The American Urological Association recommends drinking enough fluid to make at least 2 1/2 liters of urine per day.(6) For most people, this equates to drinking about 3 liters of fluid per day.
Your daily fluid goal may be different based on your body size, environment, gastrointestinal health or exercise schedule. Always ask your doctor or dietitian what fluid goal is best for you.
Mr. McStoney shows us how the more he drinks, the more urine he makes and the less concentrated calcium and oxalate molecules become. Thus, he is less likely to make a kidney stone.
What Should You Drink?
Of course, water is by far the best beverage choice. A majority of your fluid intake should be water. For many people, getting in 3 liters of water can be a challenge. Making water more “exciting” can help quite a bit. Infusing water with fruits or herbs can add a very lovely flavor without many calories or sugar. I also love unsweetened sparking water. La Croix*, Spindrift* and Bubly* are my favorite brands.
Some people find that using a “smart” water bottle helps them meet their fluid goal. The HidrateSpark* is a water bottle that actually reminds you to drink more by lighting up and tracks how much water you drink by connecting to a phone app.

Coffee and tea are okay! Be careful of how much sugar you add with table sugar, honey or flavored syrups (looking at you frappuccinos!). Yes, black tea and coffee can contain a fair amount of oxalate, but research has actually found a reduced risk of kidney stones in people who drink these beverages.(7)(8) That being said, too much caffeine can contribute to high blood pressure. And, common sense tells us the oxalate can add up if you are sipping on tea or coffee all day. Try to limit coffee and/or tea to 1-2, 8 fl oz cups per day.
It is important to avoid drinks with too much sugar. Large amounts of added sugar can increase the risk of kidney stones. I do not recommend soda, fruit juice (yes, even 100% juice), sweet tea, punch or other sweetened drinks for this reason.
2. Limit Sodium
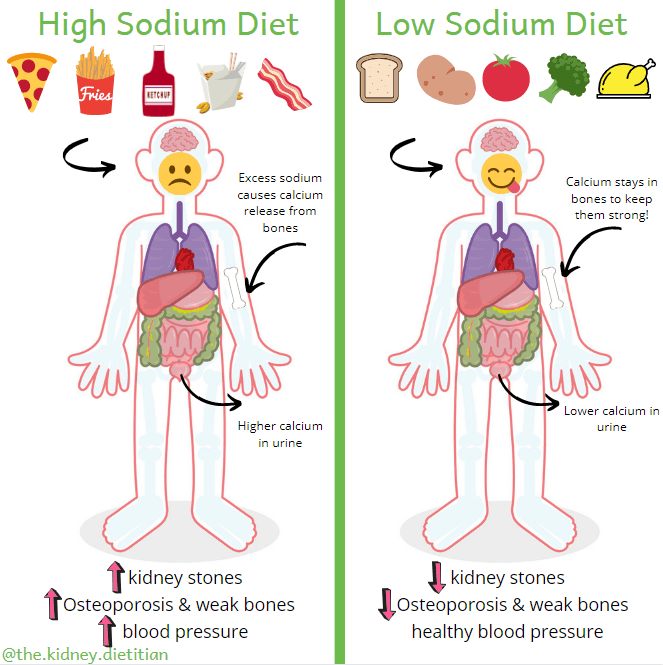
Eating too much sodium (or salt) will increase how much calcium in is your urine. (3)(9) As Mr. McStoney helps us understand, eating lots of salty foods will increase urine calcium and the risk for kidney stones. The extra calcium in the urine that comes along with a high salt diet unfortunately comes from our bones, putting them at risk as well. In addition, a high sodium diet is associated with increased blood pressure, which increases the risk of all sorts of health problems like kidney disease, heart disease, stroke and dementia.
Aim to limit sodium to 1,500-2,300mg per day. Keeping sodium to this amount is no easy task! One teaspoon salt has 2,300mg of sodium. Most Americans are eating nearly double the amount of sodium that is recommended.(10) Bread, cured meats, pizza, poultry, soups, sandwiches, cheese, mixed meat and pasta dishes and savory snacks contribute a majority of salt to the American diet.(10)
Processed Foods
Take note that a majority (about 80%) of the salt we eat is already in food. So, simply avoiding the salt shaker will not reduce sodium to our goal for most people. The key to a low sodium diet is to choose foods that are low in sodium in the first place. For the most part, this means cooking with fresh, non-processed ingredients. Restaurants, commercially prepared and to-go foods are common salty culprits as well.
3. Eat a Moderate Amount of Protein
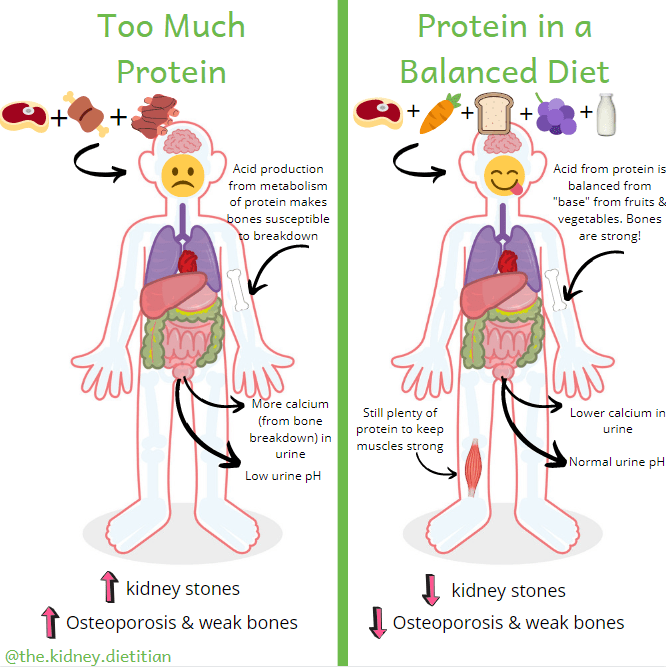
A high protein diet will increase the urine calcium.(3)(11) In addition, high protein diets produce acid during metabolism.(12) This acid is eventually excreted in our urine, which lowers urine pH and increases the risk of kidney stones.(3) Similar to sodium, the extra calcium in urine from a high protein diet is taken from bone, putting them at risk.
For most people, a healthy amount of protein is: 0.8 grams protein / kilogram body weight.(13) For example, a person who weighs 175 pounds (or 79.5 kilograms) should eat about 64 grams of protein per day (79.5kg x 0.8g/kg = 63.4g). The right amount of protein for you might be different based on your body size, age, sex or nutrition status. Always ask your dietitian what is best for you.
Similar to sodium, most Americans eat much more protein than we need.(14) The 0.8 grams per kilogram recommendation for people with kidney stones is the same amount recommended for healthy adults.(10) Even for people who are vegetarian or vegan, it is fairly easy to eat enough protein.
Unsurprisingly, most of the protein in our diet comes from meat, poultry, fish and seafood. A 3 ounce portion of animal flesh has about 25 grams of protein in it. This is 40% of the protein goal for the entire day in our example of a 175 pound person. Pair that with protein from meat eaten at other meals and the small amount of protein found in nearly all foods. You can easily see how protein adds up quickly!
Can I Eat Meat?
It is absolutely okay to have meat, but it is important to eat it in healthy portion sizes (3-6 ounces for most people). For some people, it is helpful to limit meat to only one meal per day and choose other proteins such as eggs, milk, yogurt, low sodium cheeses or whole grains at other meals. As Mr. McStoney shows us, eating protein in a healthy, balanced diet will help us keep protein portions small, and we can still feel full by filling up with all of the other, healthy food groups.
4. Eat Enough Calcium
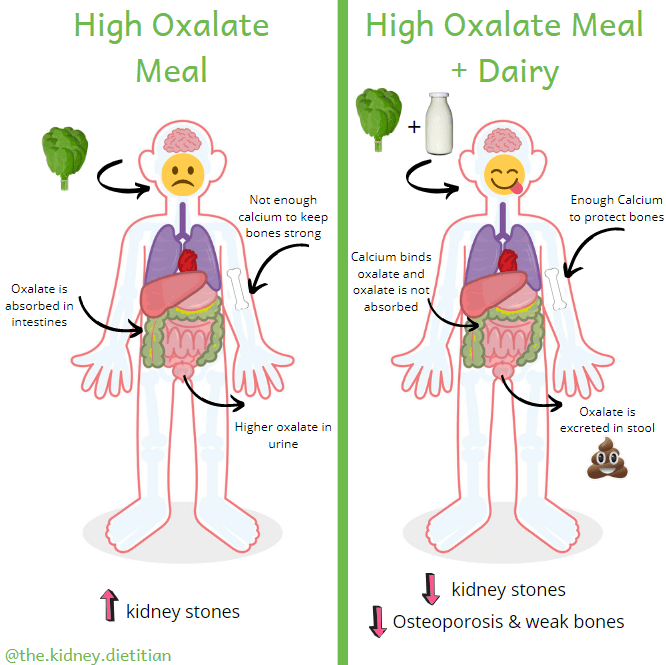
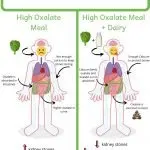
Calcium is a critically important piece of the kidney stone diet. Previously, doctors told people with kidney stones to reduce calcium and dairy. This seemed to make sense since one of our goals is to reduce urine calcium.
However, we now know about the importance of calcium in stopping oxalate absorption in the intestines. Similar to how oxalate loves to bind with calcium in our kidneys and make kidney stones, they love to bind in our intestines as well. This is great news for us! If calcium binds with oxalate before it is absorbed, the oxalate is excreted in our feces, instead of in our urine. Studies have shown nearly a 50% reduction in kidney stones by adding dairy to the diet along with the low sodium and moderate protein considerations.(15)
In addition, a diet high in calcium is critical for bone health. People who have a history of calcium kidney stones are more likely to experience bone fractures and weak bones. This makes sense, as all of that extra calcium in your urine comes primarily from breaking down bone.(16)
Mr. McStoney shows us how pairing food with dairy will stop oxalate from being absorbed and reduce the risk of kidney stones. In addition, eating enough calcium throughout the day will help protect his bones.
I’ve found this is one of the aspects of a the kidney stone diet that people struggle with the most. Understandably, people feel like drinking milk all day and eating yogurt gets rather monotonous. I created an eCookbook that aims to incorporate dairy into your meals.
How Much Calcium?
People with kidney stones should aim to eat between 1,000-1,200 mg of calcium per day. This is the same amount of calcium recommended for healthy people.(10) One serving of dairy (1 cup of milk, 3/4 cup of yogurt or 1 oz of cheese) provides around 250mg of calcium. Try to eat 3 servings of dairy per day. The dairy, in addition to small amounts of calcium from other food sources, is a good way to make sure you meet your daily calcium goal.
Food Sources of Calcium
Whenever possible, I recommend cow’s milk dairy to meet your calcium goal rather than plant sources of calcium. Good sources include:
- Milk
- Yogurt
- Kefir
- Low Sodium Cheeses (mozzarella, Swiss, ricotta, goat)
First, dairy has much more calcium in it compared to plant sources. Consider, 293mg calcium in 1 cup of milk, compared to 38mg of calcium in 1 cup of raw kale. Second, dairy has virtually zero oxalate in it, allowing all of the calcium to stop absorption of oxalate from other foods. Whereas plant sources of calcium often also contain oxalate, so the oxalate in these sources does not bind extra oxalate as well.
Calcium Timing
Timing matters! Because one of our primary reasons for eating calcium is to stop oxalate absorption, we need to eat calcium when we eat oxalate. Bottom line: make sure to eat dairy with meals. Ideally, one serving of dairy with each of your 3 meals per day. Here is an example of what your meals might look like.
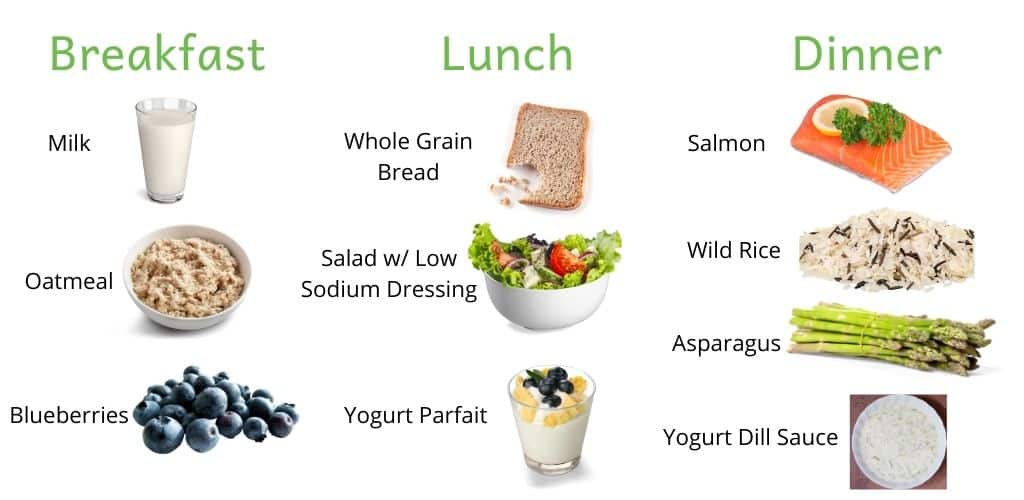
If you eat high calcium foods between meals, the calcium will certainly benefit your bones! However, it will not do a very good job of binding oxalate in the healthy fruits, vegetables and whole grains that should be a part of a healthy kidney stone diet.
Calcium Supplements & Milk Substitutes
Calcium supplements are also not ideal. Some research has shown that calcium supplements increase urine calcium more than naturally occurring calcium.(15) Milk substitutes like soy, almond, oat or coconut milk are not naturally high in calcium. Instead, these milk substitutes are supplemented with calcium to mimic cow’s milk. Therefore, they are more like taking a calcium supplement than drinking milk. I have concern for higher urine calcium as a result. However, we do need more research in this area before official conclusions can be made.
If you cannot tolerate cow’s milk or avoid it for cultural reasons, oat or rice milk are the best milk substitutes. I do recommend avoiding almond and soy milk due to concern for high oxalate. Lactaid* is also a good option for people who have a hard time tolerating cow’s milk.
Remember that calcium from supplements or milk substitutes is definitely better than no calcium at all! Work with your dietitian or doctor to figure out a plan that works best for you.
Read more about the best calcium sources for kidney stones.
5. Keep Added Sugar to a Minimum
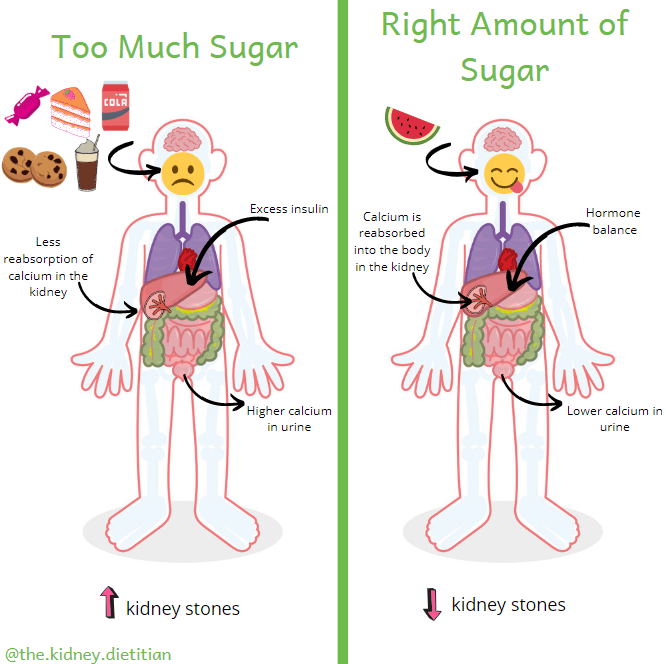
Too much sugar in your diet will increase urine calcium.(3) Therefore, sugar will increase the risk of kidney stones. In addition, high sugar intake is associated with an increased risk of heart disease and diabetes.(16)(17)
The American Heart Association recommends limiting added sugar to no more than 100 calories per day from added sugar for women. And, no more than 150 calories per day for men. This equates to no more than about 6 teaspoons (25 grams) per day for women and 9 teaspoons (38 grams) for men.
Of course, there is a lot of added sugar in desserts like cookies, cake and ice cream. Sugar-sweetened beverages are a big contributor as well. I recommend avoiding all drinks with sugar in them including regular soda, sweet tea, lemonade, punch and all juice. A single drink of any of these can easily put you over your daily added sugar goal.
Sugar sneaks into our diet via some surprising foods. You’ll find added sugar in many condiments like commercial spaghetti sauce, salad dressing or ketchup. You can also find sugar in some bread, crackers and other baked goods. Many “low sodium” products actually have sugar added to them to help boost flavor.
Fruit
Note that the recommendation is for sugar added to food, and not necessarily sugar that naturally occurs in food. Fruit often comes up in the sugar conversation. Fruit is (and absolutely should be!) a part of a healthy kidney stone diet. There certainly is sugar in fruit, however the amount is far below what you would find in sweet drinks or desserts. Also, fruit provides many healthy things like fiber and antioxidants. Importantly, fruit also is a great source of potassium. Diets high in potassium can actually reduce the risk of kidney stones, likely by increasing the pH of the urine.(o)
Bottom Line
Make sure to check the nutrition facts label for added sugar, as well as sodium. Try to find products with as little added sugar as possible. And, save sweet desserts for special occasions. Swap out ice cream after dinner for a lower sugar frozen yogurt or fruit.
6. Reduce Dietary Oxalate
Oxalate is perhaps the most tricky part of the kidney stone diet. Firstly, oxalate information found online is often conflicting, which results in frustration for people trying to follow a low oxalate diet. The oxalate food list compiled at Harvard is considered the most accurate source. I have used this information to create an oxalate list that uses standardized portions.
Foods highest in oxalate:
- Spinach (755mg per ½ cup, cooked)
- Almonds (122mg per ¼ cup) – not all nuts are high in oxalate!
- Bran (46mg per 1 cup)
- Rhubarb (31mg per ½ cup)
- Raspberries (48mg per 1 cup)
- Beets (76mg per ½ cup)
- Potato, w/ skin (97mg per potato)
- Navy beans (76mg per ½ cup, cooked)

Secondly, oxalate really is not the most important part of the kidney stone diet for most people. Research shows that a high oxalate diet is not associated with increased risk of kidney stones in the general population.(20) And, the amount of oxalate you eat does not necessarily translate to oxalate in your urine.(21)(22) This is probably because intestinal oxalate absorption and oxalate production in the liver is different from person to person.(23)(24) Focusing on increasing calcium is much more important than strictly avoiding high oxalate foods.
However, it makes sense to cut back how much oxalate you eat if you do have too much oxalate in your urine. Your doctor can order a 24-hour urine test to figure this out. How strict you need to be with oxalate restriction really depends on how much urine oxalate you have. For most people I work with, avoiding the very high oxalate foods above in addition to increasing dairy to 3 servings per day, results in healthy urine oxalate levels. However, some people do need to be more strict with the oxalate restriction. It is important to work closely with a dietitian who knows your lab values to figure out what is best for you.
Unnecessarily restricting oxalate will likely result in avoiding many otherwise very healthy foods. Most notably, whole grains are often eliminated on a low oxalate diet. Whole grains are the primary source of fiber in the American diet and cutting them out makes it very difficult to eat enough fiber. Low fiber diets are associated with an increased risk of diabetes, obesity, heart disease, hypertension, stroke, digestive health and some cancers.(9) What we eat needs to address all aspects of health. Read more about oxalate, including low oxalate snack options!
Bottom Line
Use your 24-hour urine results to determine if you need to avoid oxalate. I do recommend all people with kidney stones avoid spinach and almonds (including almond flour, butter and milk) due to the dramatically high oxalate content. Work with your dietitian to figure out what other oxalate foods are right for you.
7. Eat Lots of Fruits & Vegetables
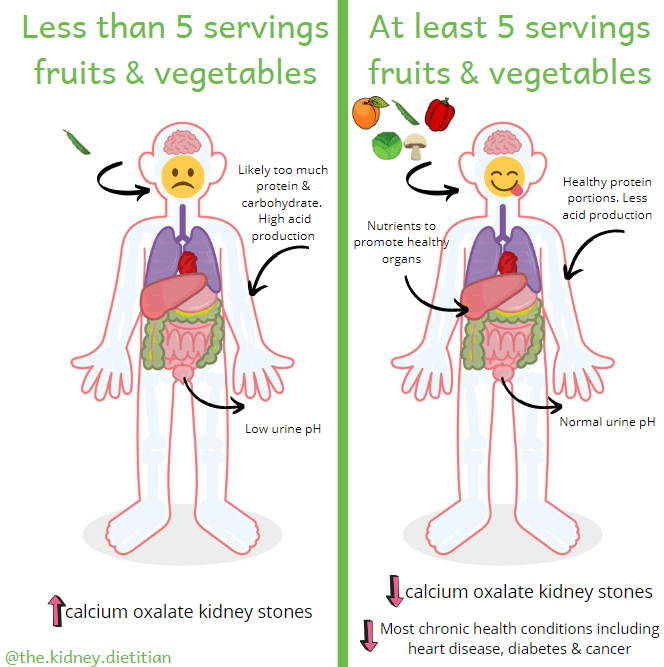
The final pillar of a healthy kidney stone diet is to eat lots of fruits and vegetables. How many? Aim for at least 5 servings per day.
Obviously, fruits and vegetables are good for us for many reasons. Eating a lot of fruits and vegetables is associated with reduced risk of hypertension, heart disease, stroke, cancer and gastrointestinal conditions.(25) For kidney stones specifically, they help make our urine less acidic. Fruits and vegetables produce alkali (or base), which helps balance acid produced from protein in our diet. Calcium oxalate kidney stones are more likely to form in acidic urine.(3)
Tips for 5 Servings of Fruits & Vegetables
- Think of every meal and snack as an opportunity to put healthy food in your body. Every meal should include at least 1 fruit or vegetable.
- Maximize your snacks. Fruit is the perfect snack as it is usually portable and pre-portioned! Veggies and hummus is another excellent option.
- Focus on making 1/2 of your plate fruits and vegetables.
- Experiment with new produce! Try a vegetable you haven’t had before. Ugli fruit anyone?
- Try preparing vegetables differently. Plain boiled broccoli isn’t very exciting. Roasting vegetables, adding tasty spices or making low sodium sauces can really elevate your usual side of plain green beans. Brussels sprouts used to have a bad reputation, but are found all over restaurant menus now!
Example Kidney Stone Diet Meals
Whew! We made it to the end. Putting all the pieces of a healthy kidney stone diet can be overwhelming. But, I promise that once you get in the swing of it, a healthy kidney stone diet is really just a healthy diet! In fact, the Dietary Guidelines for Americans aligns with the kidney stone diet perfectly! The only difference is the high fluid and low oxalate pieces of the kidney stone diet.
Here are some meal ideas to get you started:
- Butternut squash lentil salad
- Make a bowl! Top brown rice with your favorite veggies and a small amount of meat or a few beans (garbanzo tend to be the lowest in oxalate). Add some tasty low sodium sauce and you are good to go!
- Low Sodium Stir Fry
- Stuffed Peppers
- Panzanella Salad
- Homemade pizza topped with low sodium sauce and your favorite veggies
- Low sodium soups filled with lots of vegetables!
- Chicken kebobs with lots of vegetables and a side salad
Happy Eating!
Melanie
For more support for kidney stones from The Kidney Dietitian, check out my Facebook group!

Hi, Melanie. I found your site after my 4th surgery for kidney stones in 5 years (3 lithotripsy and no cystoscopy). After the 24-hour urine test, my dr. put me on calcium citrate, but I keep getting stones almost constantly. Does that mean I need more or less acid in my diet? I have severe food intolerances and can only eat 12 foods, which includes nuts and kale. I eat no added sugar or salt and no processed foods. I cannot tolerate any grains, so I use nut flour. I’m trying to down tons of water, but am at a loss as to what else I can do. Any suggestions? Thanks.
Hi Connie! I really can’t say what is best for you without looking at that complete 24-hour urine test in full and knowing a little more about your medical history and your current diet. I help people understand exactly what they should eat for stone prevention in Kidney Stone Nutrition School!
Hi Melanie: I enjoyed your article and had already implemented many of the recommendations. I was never really diagnosed with a kidney stone, I saw a Functional doctor after a very severe side pain on my right side lasting several hours. Several more of these attacks came on a regular (several months apart) basis. In 2019 I had a 24 hr urine to determine state of my kidneys along with xrays of my entire middle. The urine test showed elevated calcium oxalate and hyperoxalia. I had not caught any stones in my urine until finally something smaller than the head of a pin. Dr. wasn’t even sure it could be analyzed but they did and it was calcium oxalate in nature. Dr. put me on certain B vitamins including B12, B6 (in P-5-P form), folate and calcium citrate of 1000mg. I later switched to calcium in food and a magnesium citrate. Urologist said my stone was so small it could not possibly have created the pain and I must say, I continue with pain (not lasting as long these days if I drink water and pee) on at least a monthly/bimonthly basis, with no stones being eliminated. I had 3 episodes (the last one was yesterday), this week! I’d like to know your thoughts on the B vitamins (take/don’t take/correct amounts, etc. Also, I have just finished a book entitled “Toxic Superfoods” relating oxalate to a number of health issues. I’d like your opinion on that also if you, by chance, have seen/read any of it. Thanks for caring by sharing.
Hi Leigh! Thank you for your comment. I don’t recommend most supplements for oxalate or stone prevention due to lack of data to suggest they help. I cover all of the supplements you mention in this post. I am very familiar with that book and disagree with nearly every claim in the text. The author takes cell and animal studies and massively overstates their findings. There is no doubt that oxalate can cause issues, however there is NOT A SINGLE STUDY that has found that a low oxalate diet improves ANY of the conditions described in the book (even kidney stones!) in humans. I dive into these concepts a bit more in this post. The assumption that a low oxalate diet will improve improve the issues described is both dangerous and negligent. This assumption massively underappreciates the complexity of oxalate digestion, metabolism and excretion. Our bodies are not simple tubes with what goes in goes out. It also disregards the complexity of nutrition. A low oxalate diet will inherently be lower in many things that have been linked to actual IMPROVED health outcomes (both for general health, as well as kidney stones!).
Sorry for a bit of a rant here. I am just incredibly passionate about true evidence-based nutrition and not putting extra, unnecessary dietary restrictions on people unless there is good reason to!
Hi Melanie,
Thanks so much for this article and your website. I’m very confused, however. Pre-pandemic, I had seen a dietician in a kidney stone clinic for calcuim oxalate stones, and was also given the Harvard list. However, I came away feeling that I had to avoid most fruits and vegetables, really limiting my intake of them (especially things like avocados and oranges). We didn’t speak much about limiting protein. In fact, I seem to recall the dietician telling me to increase my protein. I was, however, told to eat calcuim with each serving of fruit/veg/grain. I feel new kidney stones building up, can’t get medical attention right now due to a backlog back of Covid, and am quite confused comparing the info on your site to what I had learned previously. I do love the idea of eating more fruit and veg, but frankly after everything, I’d learned previously, I feel kind of afraid of eating things like oranges and avocados, though I love both those foods. At this point, I no longer know what to eat. I’m wondering was the research I was given (between 2014-2017/18) based on scientific findings that have since changed. Any other tips would be appreciated. Thank you very much! Karen
Hi Karen! Thanks so much for your comment. Nutrition for everyone with kidney stones is different, so I can’t say where your dietitian was coming from. It does sound like you spent quite a bit of time focusing on oxalate. I hope this was because oxalate on your 24-hour urine test was elevated (otherwise, there really isn’t a purpose to limit oxalate). Even if you do need to limit it, it is incredibly important you still eat plenty of fruits and veggies, as being too stringent with them can actually increase your kidney stone risk! I’d love to help you sort all of this out. This is exactly what I do with my students in Kidney Stone Nutrition School.
Calcium is difficult for me as I have a milk allergy and lactose intolerance. I’ve produced about two kidney stones a year for 45+ years. Most of the recent ones were small, which I passed with no trouble or medical assistance, but I currently have a 4 mm stone, which I’m having surgery to remove. I suspect the larger stone is due to the almond creamer I was using, which I’ve recently stopped since learning more about high oxalates. It has been ages since I’ve had a 24 hour urine. I don’t remember what the numbers were. Hopefully, my new urologist will order one.
To make matters more confusing for me, my doctor put me on Atorvastatin calcium about six months ago, and I wonder if that could have a hand in this larger stone. I’ve read medical articles claiming that Atorvastatin is actually beneficial and prevents stones, but I’m skeptical. Any time I’ve ever been put on a calcium supplement (mainly during pregnancies) I’ve always created big stones.
Any suggestions?
Hello! I can’t say what is best for you without knowing more about your 24 hour urine test results. Here is some general information about calcium and stones. Although, I would highly doubt you would form a stone from almond creamer alone! I help people answer questions just like this in my course, Kidney Stone Nutrition School!
Do you have this information/ article available in Spanish?
Unfortunately I do not. I wish I did!
I have suffered with kidney stones for over 20 years. I would be okay for a year, sometimes 2 years and they would come back with a vengeance, I would have to be hospitalized, and medicated. Doctors give conflicting advice about what was causing it. They would send me for test and NEVER tell me why it was happening.
A few months ago this year I experienced the lower-tact-trifecta: kidney stones, urinary tract infection and diverticulitis. Antibiotics from the doctor and fasting for two weeks (on my own) brought me through. I was AFRAID to eat anything and loath to drink too much. I lost weight and was dehydrated (prior to this incident I was drinking over a gallon of water, via my physicians and nurses suggestion; that advice made me sicker).
Dr. Google to the rescue: I started my own search for a CURE, not just treatment and came upon your most excellent article. Your information has been a God-send. The ingredient I was missing was the Calcium. I can eat without feeling I will get sick with every mouthful. The stress was unrelenting, and I would get sick again.
Ms. Melanie, my problem is weight: I am, 62 years old and over 200 pounds I need to lose 30-40 pounds. Would you suggest reading or a diet plan.
May the Good Lord Keep Blessing You,
Your fan,
Paulette
Hi Paulette! I’m so happy that you’ve stumbled across my site and found this article helpful. I cannot say what is best for you without knowing more about your medical history and current eating habits. I help people stop stones, and address other health conditions at the same time, in my course Kidney Stone Nutrition School! I’d love to help you!
Im trying to go plant base diet due to Ckd. So doing low protein, low salt , low potassium and low phos and low oxalate coz I have high oxalate in my urine. What beans and nuts options are best for protein source and non dairy calcium sourcd?
Hello! That is a lot to juggle! My first question is always, do you really need to limit oxalate (many people with kidney stones don’t!). If you do need to, this article about calcium, and my low oxalate beans and nut articles should help. To really figure out what matters for stone prevention for you, I’d consider checking out Kidney Stone Nutrition School!
Hi Melanie. Is it a good idea to drink water infused with lemon juice to reduce the risk of calcium oxalate crystals pls? A little confused with ph levels as citric juices are acidic and the goal is to reduce the ph in kidneys to reduce binding of calcium and oxalate. Thanks for the response.
Hi Harish! Lemon juice MIGHT be helpful for calcium stones – depending on your 24-hour urine test results. Although lemon juice itself is acidic, after it is metabolized, it actually can reduce urine acid levels (just like literally ANY fruit or vegetable!). Nutrition for stones should truly 100% be based on that test – otherwise we are just sort of guessing what caused your stones and what might help prevent them. This is what I help people do in my course, Kidney Stone Nutrition School!
Interesting, I heard sodium was wrongly labelled as the ‘bad guy’, with the real issue being low potassium, calcium and other things in a nutritionally deficient diet. This seems to be how most of the keto community thinks (where I believe effects of low sodium are more pronounced).
So I’ve been eating tons of sauerkraut, cheese and things high in sodium.
Will limiting sodium really make a huge difference? (If I’m doing the rest properly?)
Everyone is different, so I can’t really say what would make a big difference for you without reviewing your 24-hour urine test. I can say that high urine calcium (the result of high sodium intake), is the most common cause of stones, so likely it would! Plus, a high sodium diet can negatively impact blood pressure, heart health, bone health and all sorts of other things. On the keto front, stones are likely so common because it is really the perfect storm. A combination of all of these things!
Hi, Melanie
LOVE this article! One tiny quibble (please forgive me — I’m a retired editor . . . ) Under Section 7, middle of the 2nd paragraph, right after citation #25, there’s this sentence: “For kidney stones specifically, they help make our acid less acidic.” Should be, of course: “they help make our URINE less acidic.” Thanks so much for all your great advice!!!
Ah! Thanks for pointing out my error, Pat. Fixed!
Hi Melanie,
What is the deal with someone with Sarcoidosis and kidney stones? Every time I increase my calcium I end up with kidney stones (4 operations so far). I also find some foods/drinks you say to avoid are contrary to what appears on your low oxalate food list ie/milk. Hoping you can clarify.
regards,
Ace
Hi Ace! Healthy eating for kidney stones is VERY different for different people, depending on what your 24-hour urine test results are, and what kind of kidney stones you have. The questions that seem to come up more often is about oxalate, but not everyone needs to limit oxalate, so, not all of my recipes are necessarily low in oxalate. I hate for people to avoid the very healthy higher oxalate foods if they don’t need to. You can learn more about that personalized approach to kidney stone nutrition here.
Hello Melanie,
Can you explain supersaturation…I’ve read several articles about it but still don’t understand it…
Thanks,
Gordon
Hi Gordon! That is a great question! You’ll probably have a supersaturation for calcium oxalate, calcium phosphate and uric acid on your 24 hour urine results. Each of these numbers basically represents a “risk” of forming that type of kidney stone. They are determined by a fancy equation that takes LOTS of information from that 24 hour urine test into consideration – ALL of the factors that could influence that stone type from forming (pH, urine volume, amount of calcium, oxalate, etc. in your urine). I talk A LOT about super saturations in Kidney Stone Nutrition School! I hope that helps!
Thank you Melanie so much for this blog and the clarity of the information presented! This is the best Kidney Stone blog I’ve found in a long long time! great research that coincides with my specialists recommendations – its just to bad I could not understand those recommendations at the time and went through a lot of pain before finding your helpful summary here.
I have had multiple reoccurring bouts with Kidney Stones (calcium oxalate stones – tested) over the last 5 years (nothing prior) and just recently developed Gout (somewhat elevated uric acid levels – 497umol/L) and have had so much trouble getting clear information about how to balance oxalates intake with calcium intake and uric acid expulsion from the body. I don’t drink, i don’t eat red meat, i dont drink pop or juice, but I do like sweets. Without a whole picture a person ends up exacerbating a problem rather than helping it.
I have recently begun transitioning more fully to a vegetarian diet due to the onset of gout and have many concerns about the increased amount of oxalates raising my risk of kidney stones – coming from many nut proteins, vegetables in general, and plant-based calcium sources. I am not a strict vegetarian and do not mind eating dairy and eggs.
2 questions…
1) In general, if one has cut their refined sugar and reduced or limited their meat intake, would it be fair to say that as long as one stays hydrated and eats enough calcium when they are in-taking higher oxalate foods that they are at a relatively low risk of making more Calcium Oxalate stones?
2.) I am having no luck finding a dietitian with your specific kind of research expertise to help navigate these conditions. I’d be grateful for any advice on how to find dietitians with who can help with specific medical conditions (Vancouver – Canada).
Thank you again!
Hi Stan! Thank you so much for your kind comment and for sharing a bit about you. I think that in general switching to a more vegetarian diet is a wonderful thing for kidney stone prevention. Just be mindful of those VERY high oxalate foods (aka spinach, almonds, rhubarb, beets & navy beans). For the vast majority of people (unless your urine oxalate is VERY high on a 24 hour urine oxalate test), this, along with adequate calcium paired with foods bring urine oxalate down to safe levels. All the benefits of those plant foods usually massively outweighs the higher oxalate intake. However, really only the results of a 24 hour urine test would be able to give you a definitive answer here.
Unfortunately, it can be very hard to find a dietitian that specializes in kidney health – and even more difficult to find one well versed in stones. The only RD I know in Canada is Emily Campbell – who is wonderful. You could also consider my online course, Kidney Stone Nutrition School, which is the closest way to work with me. I am planning the next live launch for the fall – FYI!.
I hope all of this helps!
Thank you for the reply and advice. Should I be contacting my GP for the 24 hour urine test? and if so, who should review the results?
All the best,
S
Hi Stan! Usually your nephrologist or urologist would order and review the results of that 24 hour urine test.
Thank you so much for your article, the BEST I have found regarding diet to prevent kidney stones. As you wrote, oxalate information found online is often conflicting. Your oxalate food list provides very helpful detailed information.
Hi Richard. Thank you SO very much! I’m so glad you found the article helpful!
Hi,Melanie,
Thanks for all of this valuable information!
Could you help me find a registered Dietician who is certified in kidney nutrition? I live east of Boulder, Colorado.
I want to prevent recurrence of calcium oxalate stones, have healthier bones, and still consume a healthy amount of dietary fiber. I previously had high calcium in my 24-hour urine. Oxalates weren’t tested at that time. I will soon have another 24-hour urine, but this time both calcium and oxalates will be evaluated. Should I eat my previous diet sans spinach, wheat berries, and almonds prior to that 24- hour urine? Would that tell me whether or not oxalate intake was part of the cause? I have already increased my calcium and water intake. Thank you for your help!
Cathy
Hi Cathy! I don’t know of anyone off hand that is in Colorado. I’d recommend checking out my resources page for my recommended dietitians. Also, the NKF and the Academy of Nutrition & Dietetics have decent databases of dietitians by specialty!
I was most frustrated when finding out about my need for a low Oxalate diet because I am also Celiac. The best gluten substitutes include Almond flour. Do you know if Tapioca Flour and Rice flours would be good alternatives when baking etc.? Thanks.
Either of rice or tapioca flour would be low oxalate subs! Coconut, oat, corn and chickpea flours would also all be much lower in oxalate than almond!
So much wonderful information here. Thank you for putting all of this together in an easy to read format. Everything else I have found has left me scratching my head. What would you recommend for people who do not like dairy foods (i.e. milk, yogurt, cheese, etc.)?
You are so welcome! This is EXACTLY my goal – to help people put together ALL the conflicting information out there into something that makes sense! Check out my post about calcium sources for non-dairy options!
Is bone broth good. Also what are the sources of calcium that are non dairy
Hi Donna! Thank you for your comment. I’d just be careful with the sodium in bone broth. For stones, dairy is by far the best calcium source. Fortified rice, oat and coconut milk are my next best recommendations for calcium. Hope that helps!
Melanie,
I was diagnosed with a Staghorn Calculus stone in my left kidney over 5 years ago. They didn’t want to remove it because they(the doctors) were afraid that it would further damage that kidney. I don’t know if it is oxylate or not. The urologist sees me once a year and sends me for x-rays to see if it is growing. Do you know if that particular kind of stone is oxylate?
Hi Nona! Thanks for your comment. Have you ever had a 24-hour urine test? The results from this help you (and the doctors) make a pretty good guess as to the type of kidney stone your body makes.
Lots of great info here. Very important for people to do the 24 hr urine analysis. As someone with MSK maintaining low oxalates is very important for my kidney health. I have found the Mediterranean diet and lifestyle to be the most beneficial for me.
Thank you, Kristen! That 24 hour urine test is CRITICAL to figure out the specifics of a diet that is best for you. I also love the Mediterranean diet – so many great concepts in there! And, it is delicious 🙂 Happy to hear you have found something that is working well for you.
I was told by my Urologist that I have Medullary Sponge Disease (MSK).
Thank you for your input.