Registered Dietitian approved healthy, low oxalate snacks. Along with everything you need to know about a oxalate and kidney stone prevention!
*Please note that this post contains clearly identified affiliate links. If you click on these links and choose to make a purchase, I may receive a commission (at no cost to you). As an Amazon Associate I earn from qualifying purchases.
Table of Contents
What are oxalates?
Before we dive into what foods are high or low in oxalates, it is important to understand what oxalates actually are. Don’t worry, that list of low oxalate snacks, a meal plan and food lists for oxalates are coming!
Oxalates (or oxalic acid) is a non-nutrient found naturally in many foods. Chemically speaking, oxalate is a dianion made of carbon and oxygen molecules.
Oxalate is found naturally in many foods such as almonds, most green leafy vegetables, nuts and seeds. Oxalates form in plants because they serve a critical role for the plant itself. Oxalates may help plants in calcium regulation, help protect the plant from toxic metals and even protect the plant from getting eaten by animals1.
Do we need oxalate?
Although oxalate plays an important role for plants, there is no known function for oxalate in humans. Oxalate is classified as a “non-nutrient”, or something that we eat, but does not have a function in our bodies.
So, the short answer is “no”. We do not necessarily need to consume any oxalate in our diet.
Oxalate and Kidney Stones
Oxalate is most well known for its role in the formation of kidney stones. Calcium oxalate kidney stones are by far the most common type of kidney stone. About 75% of kidney stones are formed from oxalate and calcium2. The second most common stone type is calcium phosphate, at only 12% of stones.
Many factors determine if your body will form a kidney stone. One of the biggest factors is how saturated your urine is with oxalate and calcium. The more calcium and oxalate your urine has in it, the more likely these two molecules will bind (or precipitate) and form a kidney stone.
There are three primary ways to reduce the risk of calcium oxalate kidney stones:
- Decrease how much oxalate is in your urine
- Decrease how much calcium is in your urine
- Increase how much urine you have (aka: drink more water!)
A healthy calcium oxalate kidney stone diet targets your urine risk factors. There is no single diet for kidney stone prevention. A 24-hour urine test will identify your urine risk factors.
How to Increase Urine Volume
Urine volume is the easiest thing to control. You simply need to drink fluids!
Most people with kidney stones (of any type!) should aim for 3 liters of fluid intake per day. Of course, most of this fluid should be good ol’ water. However, feel free to mix it up with unsweetened flavored waters (La Croix*, Spindrift* and Bubly* are my favorite brands) or make infused water at home with fresh or frozen fruit and/or fresh herbs.
Some people find “smart” water bottles useful to help them drink more. The HidrateSpark* water bottle actually tracks how much water you drink and reminds you to drink more by lighting up and connecting to an app on your phone.

Try to avoid drinks with too much added sugar such as regular lemonade, sweet tea, soda, punch, or fruit juice. A high sugar intake can contribute to more calcium in your urine, which is a risk factor for kidney stone formation.
How to Decrease How Much Oxalate Is In Your Urine
Eat More Calcium
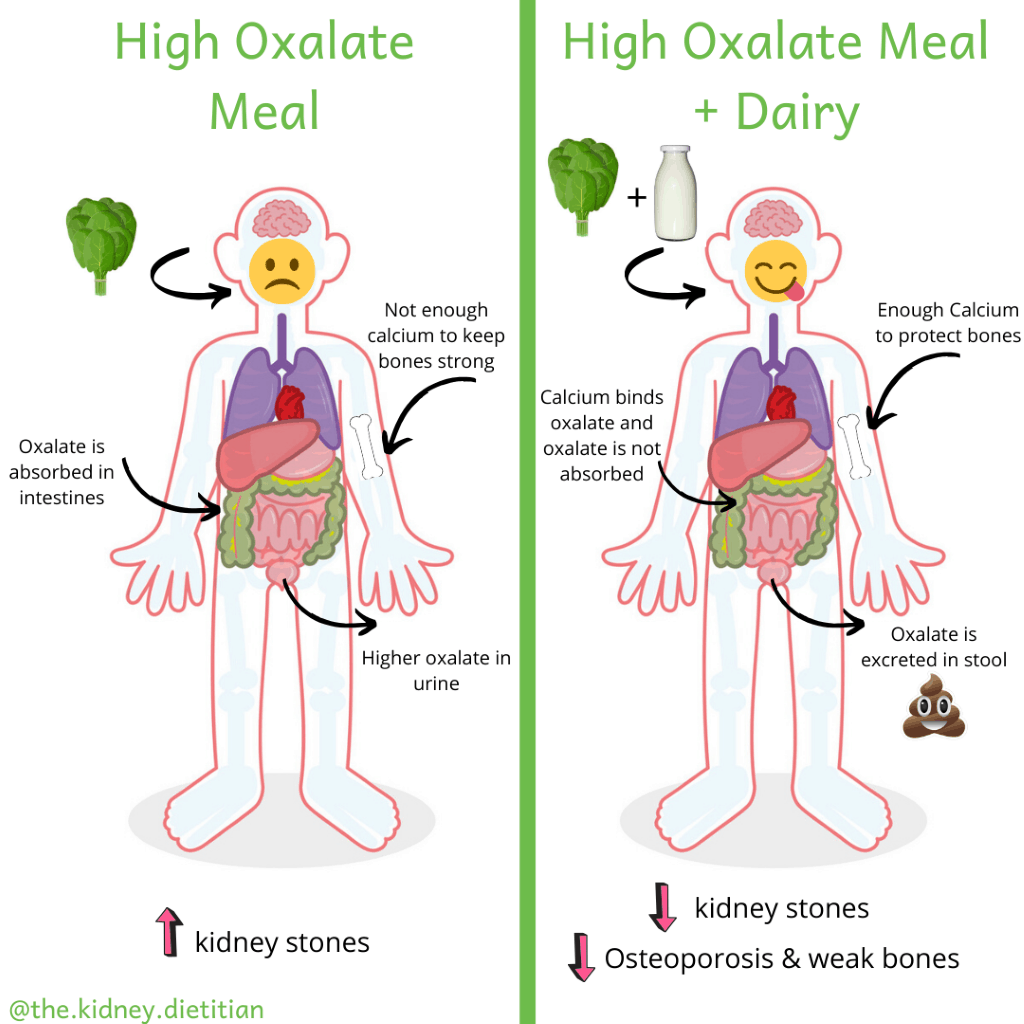
The best way to reduce oxalate in your urine is to eat more foods high in calcium. This may seem counter-intuitive. You are probably thinking: “Don’t we want to cut back how much calcium is in our urine!?” This is true, BUT calcium does a few magical things for people with kidney stones.
Firstly, calcium binds to oxalate in our intestines. This causes the oxalate to be excreted in stool and reduces how much oxalate gets absorbed into our bodies – which is great news if you have kidney stones!
Secondly, people with kidney stones are at increased risk of osteoporosis (or weak bones)3. It is very important to eat enough calcium to protect your bones.
Learn more about the best calcium sources for kidney stones.
Reduce High Oxalate Foods
The next best way to reduce oxalate in your urine is to cut back how much oxalate you eat. For many people, simply adding calcium and dairy into their diet brings oxalate down to a safe level. However, for some, they also need to cut back how much oxalate they eat.
How to Decrease How Much Calcium Is In Your Urine
This one is a little trickier. There are medications your doctor may prescribe such as thiazide diuretics to help with this. From a diet perspective, there are two factors that can help reduce calcium in urine:
- Reduce dietary sodium to no more than 2,300 mg per day.
- Avoid excess protein. This looks a little different for everyone. Work with your dietitian to figure out how much protein you need. Good general tips are:
- Enjoy meat (including beef, chicken, fish, pork, etc.) no more than once per day. For non-meat meals, choose other sources of protein such as eggs, fresh cheeses, yogurt or even beans, lentils and nuts (see chart for the best options for these foods).
- Eat meat in proper portions: 3-6oz for most people.
- Avoid excess sugar. I usually recommend limiting sugary desserts to no more than 1-2 times per week and keeping portion sizes reasonable.
My overview of a healthy diet for calcium oxalate kidney stones helps summarize all of this information.
There is no single kidney stone diet that works for everyone. I help people prevent kidney stones with a personalized, research-based and delicious approach in Kidney Stone Nutrition School!
Does Everyone Need to Limit Oxalate?
No! For most people, high oxalate foods such as almonds and spinach are healthy foods. The problem with oxalate is when there is too much oxalate in our urine, which is a risk factor for kidney stones.
Oxalate comes from two sources: our diet and the oxalate our bodies make. There are differences between people for both factors. Some people absorb a lot of oxalate from food while others do not. Some bodies make a lot of oxalate and others do not. There is a rare genetic disorder called Primary Hyperoxaluria Type 1 (PH1); PH1 causes very large amounts of oxalate to buildup in kidneys from a dysfunction in a liver enzyme responsible for breaking down oxalate4. Bottom line: not everyone is going to have too much oxalate in their urine.
Limiting dietary oxalate is not even necessary for everyone with kidney stones. The best diet to prevent kidney stones is based on the type of stone your body forms. Although most kidney stones are made of calcium oxalate, there are many other types of kidney stones including calcium phosphate, struvite, cysteine and uric acid. If you form any of these other types of stones, there is no reason to limit how much oxalate you eat as it will not reduce your risk of stones.
The best way to figure out if you have too much oxalate in your urine (and therefore, need to limit how much oxalate you eat) is a 24-hour urine test. Your nephrologist or urologist may ask you to do this test to figure out the best treatment for your kidney stones. A 24-hour urine test will quantify how much oxalate is in your urine. If it is elevated (usually more than 55 mg/day), this means you likely should cut back how much oxalate you eat.
A 24-hour urine test will measure many other stone risk factors such as: urine pH, volume, citrate, potassium, phosphate, how much protein and salt you eat and how saturated your urine is with minerals. Litholink is a common company used to perform this test5.
More about who needs a low oxalate diet.
Safely Eating High Oxalate Foods
The safest way to enjoy foods higher in oxalate is to eat foods high in calcium with meals. This will block the oxalate in foods from being absorbed, allowing you to enjoy MANY more healthy foods that may be moderately high in oxalate. Aim for 1 serving of dairy with each meal, 3 meals per day. Three servings of dairy will help you get to the recommended daily intake of calcium for adults of 1,000-1,2006. More about calcium & kidney stones.
Good dairy sources for people with kidney stones include:
- Fat free or low fat milk
- Plain low fat or fat free yogurt (try adding fruit for some sweetness!)
- Kefir
- Low sodium cottage cheese
- Low sodium cheeses
- Fresh cheeses, such as fresh mozzarella or queso fresco
- Low sodium varieties of cheese
- Cheeses naturally lower in sodium (Swiss, goat, ricotta)
Be careful of excess sodium in these dairy sources:
- Processed cheeses (Velveeta®, American cheese, nacho cheese sauce)
- Aged cheeses (Parmesan, feta, aged cheddar)
- Regular cottage cheese
If you have a hard time tolerating dairy, Lactaid* helps many people with gas and bloating.
If you struggle to fit in your 3 servings of dairy every day, check out my eCookbook! I’ve compiled low oxalate recipes that slip dairy into your diet!
Importance of Low Oxalate Snacks
It is very important to have dairy with meals. If you eat dairy between meals, the calcium will not be there to block the oxalate in the other foods you eat. This is way it is very important to eat low oxalate snacks OR be careful to incorporate dairy with your snack. For example, nuts are a common (and delicious!) snack food. Nuts tend to be higher in oxalate, but most can be safely eaten if eaten with dairy. Maybe try adding yogurt to your mid-afternoon snack of trail mix or walnuts!
Calcium Supplements
Patients often ask me about taking calcium supplements to bind oxalate instead of dairy. Unfortunately, calcium supplements increase the amount of calcium in your urine more than natural calcium found in dairy, which increases the risk of kidney stones. For people who cannot tolerate or consume dairy for other reasons, calcium supplements can reduce urine oxalate, but they are not my first choice.
Note that only cow’s milk is naturally high in calcium – all alternative milks such as soy, oat, almond, rice, etc. are supplemented with calcium as calcium does not naturally occur in these foods. Therefore, using alternative milk is essentially just like taking a calcium supplement.
Broccoli & Green Leafy Veggies for Calcium
Broccoli and some other green vegetables are surprisingly high in calcium and can be a decent source of calcium for many people. However, I do NOT recommend them as a calcium source for people with kidney stones.
Firstly, there is much less calcium in these foods compared to dairy, so we won’t get as much oxalate binding. Also, much of the calcium is already bound to oxalate in these foods, which completely negates the purpose of eating calcium block oxalate absorption.
Boiling Out That Oxalate
Boiling foods can also reduce the oxalate content. Boiling can reduce the amount of oxalate in food by more than 50%7. This may be a good option for certain high oxalate vegetables such as spinach and other greens, potatoes, okra or rutabaga.
Low Oxalate Foods
Trying to figure out which foods are high in oxalate can be incredibly frustrating. There are endless lists available online, many of which contradict each other. Unfortunately, much of this information is inaccurate. It is critical to make sure the list comes from a reliable source.
Some high oxalate foods tend to sneak into foods and we don’t even realize it! For example, many veggie burger patties may contain spinach or bran flakes. Always look at the ingredients on a food label to find those hidden high oxalate foods.
Low Oxalate Food List
| Low Oxalate (10mg or less per serving) | Medium Oxalate (11-29 mg per serving) | High Oxalate (30g or more per serving) | |
|---|---|---|---|
| Grains | Biscuits, 1 each, 6 mg Blueberry Muffins, 1 each, 9 mg Bran Muffins, 1 each, 5 mg Cheerios, 1 cup, 8 mg Cornbread, 1 piece, 4 mg Cornflakes, 1 cup, 1 mg Couscous, ½ cup, 8 mg English muffin, white, 1 each, 8 mg Oat bran, 1/3 cup, 0 mg Rice krispies, 1 cup, 3 mg Spaghetti, ½ cup, 6 mg Wheat bread, 1 slice, 5 mg | Brown rice, ½ cup 12 mg Cream of Wheat, 1 cup, 18 mg English muffin, whole wheat, 1 each, 12 mg Farina, 1 cup, 16 mg French Toast, 2 slices, 13 mg Granola, 1 cup, 20 mg Pancakes, 4 each, 11 mg | Bagel, 1 large, 40 mg Barley flour, ½ cup, 41 mg Bran cereal, 1 cup, 52 mg Bulgur, ½ cup, 43 mg Corn grits, ½ cup, 49 mg Cornmeal, ½ cup, 32 mg Millet, ½ cup, 31 mg Raisin Bran cereal, 1 cup, 46 mg Rice bran, ½ cup, 140 mg Shredded wheat cereal, 1 cup, 28 mg Soy flour, ½ cup, 47 mg Wheat berries, ½ cup, 49 mg |
| Protein | Flaxseed, 1 tablespoon, 0 mg Pecans, ¼ cup, 10 mg Pumpkin seeds, ¼ cup, 5 mg Sunflower seeds, ¼ cup, 3 mg Walnuts, ¼ cup, 8 mg | Peanuts, ¼ cup, 27 mg Pistachios, ¼ cup, 14 mg Tofu, 3.5 oz, 13 mg Veggie burger, 1 each, 24 mg | Almonds, ¼ cup, 122 mg Cashews, ¼ cup, 29 mg |
| Fruits | Apple, 1 fruit, 1 mg Apricots, 1 fruit, 0 mg Applesauce, 1 cup, 2 mg Banana, 1 fruit, 3 mg Blackberries, 1 cup, 4 mg Blueberries, 1 cup, 4 mg Cantaloupe, 1 cup, 0 mg Cherries, 1 cup, 3 mg Cranberry Sauce, ½ cup, 2 mg Figs, 1 fruit, 9 mg Grapes, 1 cup, 2 mg Honeydew Melon, 1 cup, 1 mg Lemon, 1 fruit, 4 mg Lime, 1 fruit, 3 mg Mango, 1 fruit, 1 mg Nectarine, 1 fruit, 1 mg Papaya, 1 fruit, 1 mg Peach, 1 fruit, 0 mg Pear, 1 fruit, 2 mg Pineapple, 1 cup, 4 mg Plantain, 1 fruit, 1 mg Plum, 1 fruit, 0 mg Tangerine, 1 fruit, 10 mg Raisins, 1 oz, 3 mg Strawberries, 1 cup, 4 mg Watermelon, 1 slice, 1 mg Canned cherries, ½ cup, 7 mg Canned peaches, ½ cup, 1 mg Canned pears, ½ cup, 1 mg Fruit cocktail, ½ cup, 1 mg Dried Apples, 13 rings, 2 mg Dried Apricots, ½ cup, 1 mg Dried Cranberries, ½ cup, 1 mg | Avocado, 1 each, 19 mg Dates, 1 each, 24 mg Grapefruit, ½ fruit, 12 mg Kiwi, 1 fruit, 16 mg Orange, 1 fruit, 29 mg Dried figs, 5 each, 24 mg Dried prunes, 5 prunes, 11 mg | Raspberries, 1 cup, 48 mg Canned pineapple, ½ cup, 24 mg Dried pineapple, ½ cup, 30 mg |
| Vegetables | Alfalfa sprouts, ½ cup, 0 mg Artichoke, 1 heart, 5 mg Asian mixed vegetables, ½ cup, 6 mg Asparagus, 4 spears, 6 mg Bok choy, 1 cup raw, 1 mg Cabbage, ½ cup, 1 mg Carrots, ½ cup cooked, 7 mg Cauliflower, ½ cup cooked, 1 mg Celery, ½ cup cooked, 5 mg Chili peppers, ½ cup, 5 mg Chives, 1 teaspoon, 0 mg Collard greens, ½ cup cooked, 5 mg Corn, ½ cup, 1 mg Cucumber, ¼ each, 1 mg Endive, ½ cup, 0 mg Green beans, ½ cup, 9 mg Green pepper, ½ cup, 5 mg Iceberg lettuce, 1 cup, 0 mg Kale, raw, 1 cup, 2 mg Mixed vegetables, ½ cup frozen, 5 mg Mung beans, ½ cup, 8 mg Mushrooms, 1 each, 0 mg Mustard greens, 1 cup raw, 4 mg Onion, 1 small, 1 mg Peas, ½ cup, 1 mg Tomato, 1 each, 7 mg Radish, 10 each, 0 mg Romaine lettuce, 1 cup, 0 mg Scallions, ½ cup, 1 mg Sea vegetables, 1 cup, 3 mg Water chestnuts, 4 each, 0 mg Yellow squash, ½ cup, 4 mg Zucchini, ½ cup, 1 mg | Bamboo shoots, ½ cup, 18 mg Broccoli, 1 cup raw, 12 mg Brussels Sprouts, ½ cup, 17 mg Carrots, ½ large raw, 15 mg Fava beans, ½ cup, 20 mg Kidney Beans, ½ cup, 15 mg Olives, 10 each, 18 mg Parsnip, ½ cup, 15 mg Potato chips, 1 oz, 21 mg Potatoes, mashed, ½ cup, 15 mg Refried beans, ½ cup, 16 mg Sweet potatoes, ½ cup, 14 mg Tomato sauce, ½ cup, 17 mg | Beets, ½ cup, 76 mg Navy beans, ½ cup, 76 mg Okra, ½ cup, 57 mg Potato, baked w/ skin, 1 each, 97 mg Potatoes, French fries, ½ cup, 51 mg Rhubarb, ½ cup, 541 mg Rutabaga, ½ cup, 31 mg Soybeans, ½ cup, 48 mg Spinach, ½ cup cooked, 755 mg Spinach, 1 cup raw, 656 mg Turnip, ½ cup, 30 mg Yams, ½ cup, 40 mg |
| Snacks | Popcorn, 1 cup, 5 mg Pretzels, 1 oz, 5 mg Ritz crackers, 5 crackers, 3 mg Saltines, 5 crackers, 5 mg Tortilla chips, 1 oz, 7 mg Triscuits, 5 crackers, 5 mg Wheat crackers, 5 crackers, 5 mg | Potato chips, 1 oz, 21 mg | - |
| Desserts | Chocolate pudding, ½ cup, 2 mg Custard, ½ cup, 0 mg Fig bar, 1 cookie, 4 mg Fruit roll up, 1 roll, 2 mg Graham cracker, 1 sheet, 2 mg Jello, 1 cup, 1 mg Milk chocolate candy, 1 oz, 5 mg Oatmeal cookie, 1 cookie, 3 mg Pie, 1/8 pie, 5 mg Popsicle, 1 each, 0 mg Pudding popsicle, 1 each, 5 mg Rice cake, 1 cake, 2 mg Rice krispie treat, 1 bar, 1 mg Sherbet, ½ cup, 0 mg Snack cake, 1 cake, 3 mg Vanilla pudding, ½ cup, 0 mg | Cake, 1 oz, 15 mg Chocolate chip cookie, 1 medium, 10 mg | Brownie, 1 oz, 31 mg Candy with nuts, 1 piece, 38 mg Chocolate syrup, 2 tablespoons, 38 mg Stevia artificial sweetener, 1 packet, 42 mg |
| Beverages | Apple juice, 1 cup, 2 mg Apricot juice, 1 cup, 2 mg Beer, 12 oz, 4 mg Chocolate milk, 1 cup, 7 mg Coffee, 1 cup, 2 mg Gatorade, 1 cup, 0 mg Grape juice, 1 cup, 1 mg Grapefruit juice, 1 cup, 0 mg Kool-Aid, 1 cup, 1 mg Liquor, 1 oz, 0 mg Mango juice, 1 cup, 1 mg Milk, 1 cup, 1 mg Orange juice, 1 cup, 2 mg Pineapple juice, 1 cup, 3 mg Prune juice, 1 cup, 7 mg Soda, 1 cup, 0 mg Wine, 4 oz, 1 mg | Black tea, 1 cup, 14 mg Carrot juice, 1 cup, 27 mg Lemonade, 1 cup, 15 mg Rice milk, 1 cup, 13 mg Soy milk, 1 cup, 20 mg Tomato juice, 1 cup, 14 mg | Hot chocolate, 1 cup, 65 mg |
| Condiments & Other | Apple butter, 1 tablespoon, 0 mg Butter, 1 tablespoon, 0 mg Cream cheese, 1 oz, 1 mg Cream sauce, ¼ cup, 0 mg Gravy, ¼ cup, 1 mg Horseradish, 1 tablespoon, 0 mg Jam/jelly, 1 tablespoon, 1 mg Ketchup, 1 packet, 1 mg Mayonnaise, 1 tablespoon, 0 mg Mustard, 1 teaspoon, 1 mg Salsa, 1 tablespoon, 1 mg Soy sauce, 1 tablespoon, 3 mg Syrup, 1 tablespoon, 0 mg Whipped cream, 2 tablespoon, 0 mg | Peanut butter, 1 tablespoon, 13 mg Tahini, 1 tablespoon, 16 mg | Miso soup, 1 cup, 111 mg |
All dairy (milk, yogurt, cheese) and animal proteins (chicken, turkey, fish, seafood, beef, pork, etc.) are low in oxalate.
How Much Oxalate Can I Eat?
This really depends on your urine oxalate levels. For many people, simply adding a serving of dairy to your diet will cause urine oxalate levels to come tumbling down. Other people require more strict dietary restriction of oxalate to see normal urine levels.
For most patients, I DO NOT recommend strictly following this list or trying to count how much oxalate they eat. Doing this will unnecessarily cut out many healthy foods and, lets face it, isn’t fun at all! Instead, it is best to work with your doctor track how much oxalate is in your urine after you increase dairy and take out those very high oxalate foods.
For you numbers people, it is reasonable to limit oxalate to 200mg/day. Some may need more severe restriction down to 100mg/day.
Low Oxalate Meal Plan
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | |
|---|---|---|---|---|---|
| Breakfast | 1 cup oatmeal made with skim milk ¾ cup blueberries 2 tablespoons unsalted walnuts 1 cup coffee w/ 1 Tbs cream & 1 tsp sugar | 1 boiled egg 2 slices whole wheat toast w/ 2 teaspoons margarine 1 banana 1 cup skim milk 1 cup coffee w/ 1 Tbs cream & 1 teaspoon sugar | 1 cup cornflakes 1 cup sliced strawberries 1 cup skim milk 1 cup coffee w/ 1 Tbs cream & 1 tsp sugar | 1 scrambled egg with 1 oz mozzarella cheese 1 slice whole wheat toast w/ 1 tsp ½ cup canned peaches ½ cup orange juice 1 cup coffee w/ 1 Tbs cream & 1 tsp sugar | ½ cup plain low-fat yogurt ½ cup mandarin oranges 1 slice whole wheat toast w/ 1 tsp margarine 1 cup coffee w/ 1 Tbs cream & 1 tsp sugar |
| Lunch | Low Sodium Turkey Sandwich w/ whole wheat bread, 2 oz low sodium turkey, lettuce, tomato, 1 slice swiss cheese & 1 tablespoon mayo 1 cup baby carrots 1 small bag unsalted pretzels 1 cup skim milk | 3 cups salad w/ ½ cup black beans, mixed greens, cucumbers, carrots, onions & 1 tablespoon oil/vinegar dressing 1 whole wheat roll with 2 tsp margarine 1 pear 1 cup skim milk | 1 cup low sodium chicken noodle soup with carrots & celery 1 slice whole wheat bread w/ 2 tsp margarine 1 cup melon 1 cup skim milk | 2 small tacos with roasted poblano peppers & onions, lettuce, tomato, onion and 1 Tbs sour cream ½ cup corn ½ cup brown rice 1 cup skim milk | Egg salad sandwich with whole wheat bread 1 cup cucumber slices w/ 1 Tbs oil & vinegar dressing 1 apple 1 cup unsweetened iced green tea |
| Dinner | 2 oz whole wheat pasta with cottage cheese sauce and roasted asparagus 1 cup arugula salad with walnuts, tomatoes & balsamic vinegar 1 cup sugar free lemonade | 2 cups Indian veggie curry made with cauliflower, green beans, onion, chicken and plain yogurt ½ cup brown basmati rice | 3 oz broiled tilapia w/ lemon 1 cup brown rice 1 cup green beans w/ 1 tsp margarine ½ cup sorbet 1 cup skim milk | 3 oz grilled chicken ½ cup green peas ½ cup egg pasta Romaine salad w/ 2 tsp oil & vinegar dressing 1 cup skim milk | 3 oz baked salmon 1 cup sautéed kale w/ garlic and 1 tsp olive oil and garlic ½ cup wild rice 1 whole wheat dinner roll w/ 1 tsp margarine ½ cup chocolate pudding 1 cup skim milk |
| Snack | 1 orange | ¾ cup low-fat plain yogurt with ½ cup mixed berries | ¼ cup unsalted trail mix | ½ grapefruit | 2 cups low sodium popcorn |
Click here for a PDF of this meal plan.
Low Oxalate Snacks
Some great ideas for low oxalate snacks:
- Fruit! Fruit is the perfect snack as it is portable and most are already in the perfect portions. Grab an apple, orange, banana, plum, peach, bunch of grapes or a nectarine.
- We know how important dairy is for most people with kidney stones, so using a snack as an excuse to get in dairy is perfect! Mix plain yogurt with blueberries or your favorite fruit.
- Homemade trail mix. Make your own trail mix to make sure you are choosing low oxalate ingredients. Try combining dried apricots, dried cranberries, unsalted walnuts and unsalted sunflower seeds. You could even throw in a few M&Ms for an extra treat! Check out my low oxalate trail mix recipe.
- Low sodium crackers and fresh cheese. Try Hint of Salt Triscuits* (only 50mg per 6 crackers!) or Hint of Salt Wheat Thins* with fresh mozzarella.
- Popcorn made from kernels on the stovetop or with an air-popper. Microwave or pre-popped popcorn can be full of added sodium and fat. Making it at home allows control over these ingredients. Use just a pinch of salt or experiment using dried herbs and spices to flavor your popcorn. If you prefer commercial popcorn, Skinny Pop* is my favorite road trip snack!
- Low sodium pretzels. Try Snyder’s of Hanover Unsalted Mini Pretzels* (0 mg of sodium per 19 minis!)
- Raisins or other low oxalate dried fruit. Try dried apples, cranberries, strawberries, apricots, mango or peaches. Be careful of portion size here!
- Harvest Snaps* – these pea pods are made into a tasty, low sodium snack!
Other Oxalate Considerations
Vitamin C and Oxalate
Large doses of vitamin C may contribute to extra oxalate in urine. Oxalate is a byproduct of vitamin C metabolism. There are cases of very high vitamin C supplementation causing excessive amount of oxalate in urine and kidney damage8.
It would be difficult to ingest excess vitamin C from food, but very easy to do from supplements. Most multivitamins have at least 100% of your daily vitamin C. In addition, you might be getting vitamin C from supplemented orange juice, breakfast cereals, cough drops and supplements such as Emergen-C®. It adds up quickly!
As always, it is best to get vitamins and minerals from food instead of supplements. This is easy to do for vitamin C if you are eating the recommended 5 servings of fruits and vegetables per day. One orange or bell pepper has almost your entire day’s worth of vitamin C.
Probiotics and Oxalate
Did you know the bacteria in our intestines can impact oxalate too? Oxalobacter formigenes (O. formigenes) is a bacteria in our gastrointestinal tract and part of our microbiome. O. formigenes breaks down oxalate from food in our intestines.
Studies have shown that antibiotics can reduce the amount of O. formigenes in our intestines. Less of the bacteria can lead to higher absorption of oxalate and subsequent higher urine oxalate9. However, more research needs to be done to figure out if supplementing O. formigenes with a probiotic causes a decrease in urine oxalate. Probiotics are not a proven treatment for kidney stones at this time.
Summary
In summary, oxalate can be a tricky thing for people with kidney stones. Those with high urine oxalate should be careful to avoid foods very high in oxalate (spinach, almonds, beets and rhubarb). It is also very important to eat dairy with meals to block oxalate absorption and help with bone health.
For other resources about a low oxalate diet:
Check out information from The University of Chicago or Cleveland Clinic.
Peruse my low oxalate recipes.
Consider joining my Kidney Stone Facebook Community on Facebook.
Happy Eating!
Melanie
References
- Nakata PA. Advances in our understanding of calcium oxalate crystal formation and function in plants. Plant Sci. 2003;164(6):901-909. doi:10.1016/S0168-9452(03)00120-1
- Worcester EM, Coe FL. Nephrolithiasis. Prim Care Clin Off Pract. 2008;35(2):369-391. doi:10.1016/j.pop.2008.01.005
- Carbone LD, Hovey KM, Andrews CA, et al. Urinary Tract Stones and Osteoporosis: Findings From the Women’s Health Initiative. J Bone Miner Res Off J Am Soc Bone Miner Res. 2015;30(11):2096-2102. doi:10.1002/jbmr.2553
- Primary hyperoxaluria type 1 | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. https://rarediseases.info.nih.gov/diseases/2835/primary-hyperoxaluria-type-1. Accessed March 29, 2020.
- Home | Litholink. https://www.litholink.com/. Accessed March 29, 2020.
- Office of Dietary Supplements – Calcium. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/. Accessed March 29, 2020.
- Shi L, Arntfield SD, Nickerson M. Changes in levels of phytic acid, lectins and oxalates during soaking and cooking of Canadian pulses. Food Res Int. 2018;107:660-668. doi:10.1016/j.foodres.2018.02.056
- Lamarche J, Nair R, Peguero A, Courville C. Vitamin C-Induced Oxalate Nephropathy. International Journal of Nephrology. doi:https://doi.org/10.4061/2011/146927
- Siener R. The role of Oxalobacter formigenes in calcium oxalate stone disease. https://books.publisso.de/en/publisso_gold/publishing/books/overview/52/5. doi:10.5680/lhuii000001

Hi, I have a question about Vitamin C “supplements” is this the typical ascorbic acid? What about getting natural Vitamin C from Amla berry, Camu Camu berry and Acerola Cherry? Would that cause high urine oxalate?
We don’t worry about vitamin C that occurs naturally in any food!
Thank you so much for your weigh-in. Think I need to clarify, this isn’t from eating the actual whole fruits, this is from drinking the organic FREEZE-DRIED POWDERS acerola cherry, amla and camu camu disolved in water or smoothie. Another question I had re homemade cashew milk – i like to use it to make creamy sauces without the fat of heavy whipping cream. Would boiling my cashews be helpful for significant oxalate reduction?
Got it! It would probably be preferable to eat them in whole food form. But, the freeze dried powder is probably ok. I’d have to look at your 24 hour urine test and understand more what your entire diet looks like to be able to give a good answer. I almost never recommend boiling food to reduce oxalate because it also reduces ALL other water soluble nutrients.
Hi Melanie,
Thank you for all this information/blog. I have had a couple bouts with Kidney stones and currently have 1 in each kidney about 6mm and 7mm.
Urologist gave me printed out info regarding what to eat and what not to eat as far as low oxalates, med oxalates, and high oxalates which I have to agree with you; the information is confusing and somewhat contradicting.
I have not had my levels tested…would love to do that and will look into how to go about it.
The Urologist told me to add 4oz of Citric Acid to my daily water intake…so we basically are squeezing fresh lemons and limes and that juice is what I add to my water. What I don’t know is if drinking that much Citric Acid is causing anything detrimental to my health.
He also told me to drink 2-3 servings of Milk a day. What I read here is that the Milk should be WITH my meal not prior to eating or 2 hours after I have ate.
I also read about spices…my husband and I love to cook and very rarely eat out. Our fat in cooking generally is Olive Oil…sometimes a small sliver of butter for flavor. If I use butter, I lessen the salt. Salt we use is Trader Joes Onion Salt Blend. Is this ok?
I read that Black Pepper is very high in oxalates and I should switch to white pepper. Really?
We use fresh garlic with all our meals…on the heavy side. Is this something I need to decrease?
When we make spaghetti, I take fennel seed and grind it to a powder and then use probably 1 tablespoon in my sauce. Do I have to remove this from my cooking? I saw fennel seed was a high oxalate.
Another meal we do is chile verde with pork shoulder. We roast the tomatillos, onions, jalapenos, poblano, and anaheims…then we will make burritos that have a mixture of white rice, black beans, green chilis and a small amount of shredded mexican cheese blend…we then top the chile verde with pork shoulder and bake.
I read that most of the ingredients…black beans, green chilis, cumin, chili powder are high in oxalates so I can’t have this meal any more?
Hi Jenny! I’m so glad you are here! I cannot stress how important that 24-hour urine test is. Without it, we have NO idea what you should be doing to prevent stones. Your doctor is making all sorts of assumptions by giving you dietary advice without that test. For ALL spices, I say they are totally fine to use in cooking. The amount of oxalate you’ll realistically get from spices in cooking in minimal. Supplements is where I start to get concerned. Let us know if you have any questions about the test!
Hello Melanie.
I appreciate you knowledge on the matter of Kidney stones and I use this knowledge daily. Thank you for this Blog!
Several articles state that calcium supplements are not beneficial.
What does your knowledge say about a liquid, Plant-based Algae supplement?
There is no research to compare different types of calcium supplements. IF you have high urine calcium, I’d steer clear of ANY type of calcium supplement.
Hi Melanie. Thank you so much for everything you do and post! I was told I do NOT have to avoid oxalates, but do not overdo chocolate and spinach…… 2 of my favorite things…. This was after they examined the stone and 24-hour collection. I primarily have to make sure I drink a LOT of water every day. However, I decided to focus on foods with lower oxalate anyway. Before my kidney stone incident over Christmas, I had ordered a Joyoung soy milk maker, only to discover AFTER the incident that there are sooo many different opinions on Oxalate levels in soymilk since 2001. I am not sure how to measure the oxalate count for 1/3 cup soy beans making 34ml of soy milk and then strained after I make the milk in the machine. I stopped buying commercial soy milk because I wanted healthier soy milk. Any thoughts on this? Thank you!
Hi Jinny! This post about oxalate in plant based milks should be helpful to you! This is the most recent info I have on their oxalate content.
I would caution using a low oxalate diet – it often lacks many GOOD things for stone prevention such as magnesium and phytate. Just my thoughts!
Melanie,
Thank you so much! I hope you don’t mind me sending a cyber hug! My mom thanks you too.
I am so grateful for your help.
Jinny
I don’t have high uric acid levels (tested many times and it is always on the low end). This is why my previous doctor, in 2012 determined that I have PSEUDO gout caused by oxalates.
No, I don’t supplement with vitamin C. But does Ca citrate and Mg citrate cause an increase of vitamin C? Does the citric acid in those forms get converted into vitamin C? I’m not a scientist.
I have read that calcium oxalate crystals can get into the joints. This is why I have been trying to eat low oxalate foods.
Many thanks again.
Interesting. I’d be interested to understand how and why your doctor diagnosed you with oxalate caused gout. There is no data to suggest oxalate could cause gout. Citrate does not get converted to vitamin C. Citrate is actually a really good thing for stone prevention. There is no research that a low oxalate diet will help reduce oxalate crystals in joints or help/prevent arthritis.
Pseudogout is formally known as calcium pyrophosphate deposition disease or CPPD. But the condition is commonly called pseudogout because of its similarity to gout. In both pseudogout and gout, crystal deposits form within a joint, although the type of crystal differs for each condition.
https://pubmed.ncbi.nlm.nih.gov/15821508/
Purpose: We determined why calcium oxalate stones instead of uric acid stones form in some patients with gouty diathesis.
Conclusions: Calcium oxalate stones may form in some patients with gouty diathesis due to increased urinary excretion of calcium and reduced excretion of citrate. Relative hypercalciuria in GD + Ca may be due to intestinal hyperabsorption of calcium.
This is why I am taking the citrates.
Thank you! I am aware of this. However, there is still no data to suggest that a low oxalate diet will help this condition. I fear it would actually limit many foods we know are GOOD for gout (in general) prevention and things that we know that inhibit calcium oxalate kidney stones. This is especially true if we don’t know the cause of your crystals – often high calcium is more the concern.
Thank you Melanie!
It is really hard to figure out what I should be doing for pseudogout. Even the doctors don’t have a solution.
Allopurinol doesn’t work for pseudogout. I had a doctor prescribe that and it did nothing.
I really appreciate all of your insights.
Happy to help!
Thank you for such a thorough explanation on oxalates. I don’t supplement vitamin C but this calcium reference in with the vitamin C info doesn’t make sense to me; “One orange or bell pepper has almost your entire day’s worth of vitamin C. If you do choose to take supplements, I recommend limiting supplemental CALCIUM to no more than 500 mg/day.”
Oddly enough, I don’t have kidney stones, but have pseudo gout caused by oxalates. This was determined by my doctor in 2012. She only told me to stop eating spinach (haven’t ate it since 2012) which is what gave the worst gout attack I had ever had.
Since my husband is fighting cancer we are on the WFPB diet and it is working for him. Eliminating dairy for me was the best thing I have done for my arthritis. Within 3 weeks of not eat any dairy my arthritis greatly improved. Even my sinuses got better.
I have been adding calcium citrate in powder form with my meals, 1/4 tsp in either my beverage or mixed in my food. I am also taking Mg Citrate just before bed. Also, some K Bicarbonate with the calcium citrate and I am adding 1/4 tsp to a gallon of water.
I have eliminated the high oxalate foods but it is hard because, some foods haven’t been tested for oxalates.
Would you recommend this low oxalate diet for my pseudo gout? I can’t seem to find any references or studies on pseudo gout and oxalates.
Thank you so much!
Hi Shelley! Thank you for your comment. That bit on supplements is an error. I’m correcting it now. I’d actually recommend completely avoiding vitamin C supplements if you have high urine oxalate. And no, I cannot recommend a low oxalate diet for gout. There is no research to back up this recommendation. In fact, diets that have A LOT of plant foods are shown to be most beneficial for gout and lowering uric acid levels. I’d fear a low oxalate diet could actually make gout worse.