The phrase “renal diet” may be one of the most confusing in the nutrition world. If you Google it, you will find endless lists of foods to avoid. These lists and advice are often conflicting, which can be confusing and frustrating.
You may even find websites that claim foods or regimens will “cure” kidney disease. This is completely bogus 99% of the time, and these recommendations can be dangerous to people with kidney disease. I’d steer clear of sites making claims like these.
Read on to understand what a renal diet is and what it means for you.
What Does a “Renal Diet” Mean?
“Renal” is simply a fancy word for “kidney”. In the medical world, kidney has many different names including “renal” and “neph”. For example, the formal title for your kidney doctor is a “nephrologist”.
So, a renal diet is a diet that is good for kidneys. The kicker is, there is no single renal diet that is right for everyone. A healthy renal diet for you is very dependent on what kind of kidney disease you have, what your kidney function is, and what your other labs look like.
Know that there is no single food that will cure or prevent progression of kidney disease. A healthy renal diet must focus on whole diet patterns instead of eating (or limiting!) single foods.
A Renal Diet is Different For Everyone!
Some of the “renal diet” confusion comes from the fact that a kidney friendly diet is not the same for everyone. For example, a renal diet for someone with early stages of kidney disease is very different than a renal diet for the later stages of disease.
To complicate things further, both of those diets are different than a renal diet for someone who is on dialysis or has a history of kidney stones. No wonder everyone is confused!
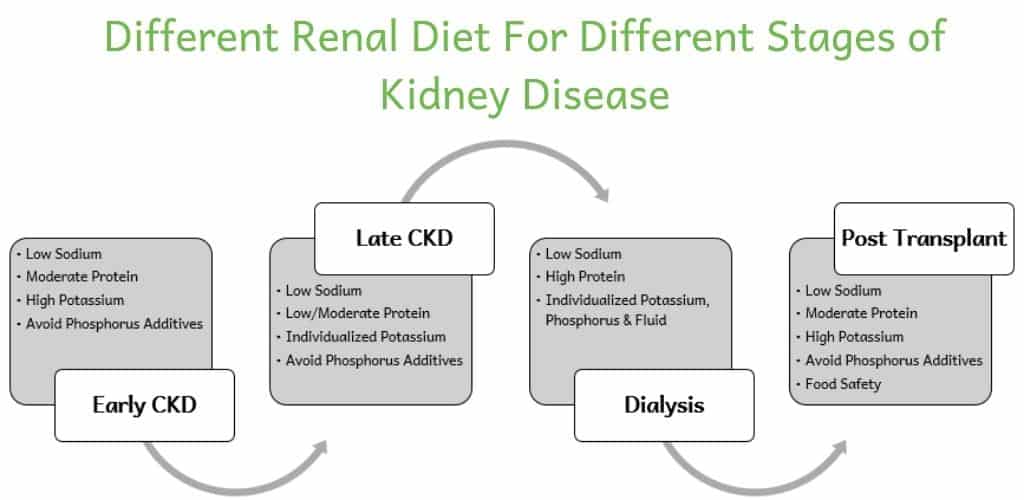
Here is an overview of how the recommendations for a renal diet differ. This will help you learn what a renal diet is for you.
What Is a Renal Diet for Chronic Kidney Disease?
A renal diet for Chronic Kidney Disease (CKD) changes drastically depending on the stage of CKD you have. I’ll walk you through each aspect of a renal diet for CKD and help you understand how needs change.
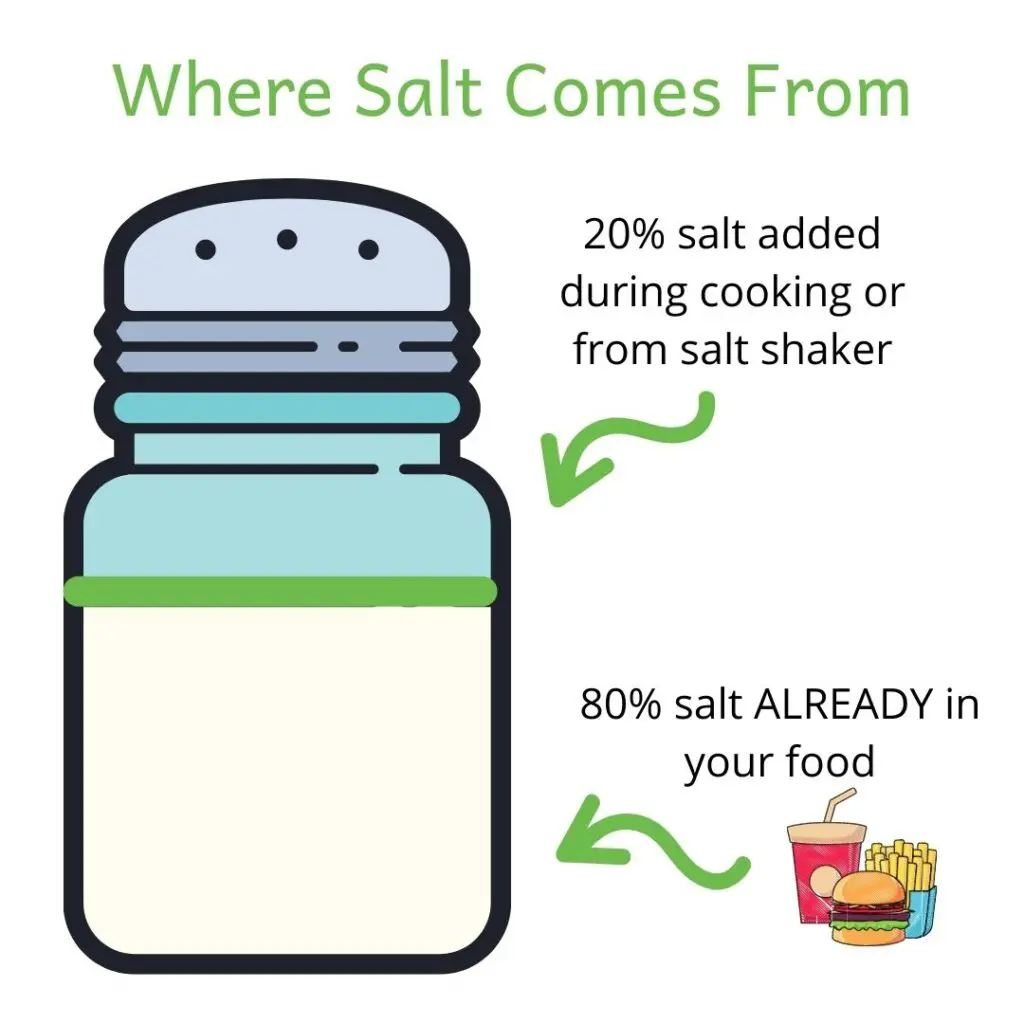
Sodium
For all stages of kidney disease, sodium should be limited to 1,500-2,300mg per day on a renal diet. (1) This helps control blood pressure (which is key to preventing more kidney damage!) and swelling.
Keeping sodium in check can also help lower the amount of protein in your urine.
Protein
In CKD stage 1-3a (or, a GFR of 45ml/min or more), a healthy renal diet is moderately low in protein. Most people should aim for 0.8 grams of protein per kilogram body weight per day in these early stages. This is plenty of protein to maintain or build muscle!
If CKD progresses to stages 3b-5 (or, a GFR less than 45ml/min), protein recommendations go down. For this stage, the National Kidney Foundation recommends a protein intake between 0.55-0.6 g/kg body weight. (1)
Of note, people who have both diabetes and CKD should not limit protein this much. Aim for 0.8 g/kg body weight if you have diabetes. (1)
On dialysis, protein needs increase. A diet high in protein is important to maintain muscle and prevent poor nutrition in people on dialysis. Protein recommendations go up to 1.2 grams of protein per kilogram body weight per day for people on dialysis. (1)
Protein needs are tricky and may be different based on your body size, nutrition status, medical history, and age. Ask your dietitian how much protein is right for you!
Potassium
On a renal diet, dietary potassium only needs to be limited in people with high blood potassium. In the early stages of kidney disease, blood potassium levels are usually normal! In fact, a diet high in potassium can help control blood pressure and protect your kidneys. (2)
If kidney disease progresses to stage 4 or 5, high blood potassium levels (aka hyperkalemia) are more common. The kidneys are not able to get rid of potassium as well. Potassium can build up in your body and, in severe cases, cause serious issues like heart arrhythmias. If your blood potassium level is high, then cutting back how much potassium you eat is a good idea. (1)
Phosphorus
Artificial phosphorus should be limited for nearly everyone with kidney disease, no matter the stage.
High levels of phosphorus can cause bone disease, heart disease and even faster progression of kidney disease.
Natural sources of phosphorus, such as in whole grains, beans, nuts, seeds, and lentils, usually do not need to be restricted until very advanced CKD (if ever). This is especially true if phosphorus from animal products is avoided and plant proteins are used in place of meat, chicken and fish at meals.
Natural phosphorus is poorly absorbed, so does not have as big an impact on phosphorus levels as artificial phosphorus does. (3)
Dietary Acid Load
Reducing dietary acid load is the most important thing you can do nutritionally to slow the progression of kidney disease. (4)
Dietary acid load primarily comes from animal protein. Fruits and vegetables help neutralize acid. This is why it is so important that any renal diet include PLENTY of fruits and veggies, no matter the stage!
Aim for at least 5 servings of fruits and vegetables every day.
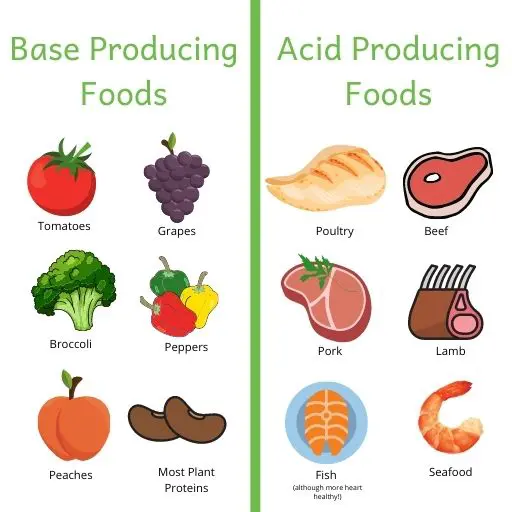
Plant proteins produce significantly less acid than animal proteins. Eating more plant proteins like nuts, seeds, lentils, whole grains, and beans in place of animal proteins can slow CKD progression.
Learn more about dietary acid load and PRAL.
Fluid
Both dehydration and not drinking enough fluid can hurt kidneys. However, most people with kidney disease do not need to limit fluid unless kidney disease is very advanced. Most people on a renal diet for kidney disease should drink about 2 liters of water each day.
However, people with some health conditions may need to limit fluid. Here are some examples:
- Dialysis
- Advanced stages of CKD
- Heart failure
- Liver failure
Fluid needs on a renal diet are tricky! Ask your doctor how much fluid is right for you.
What Is a Renal Diet for Polycystic Kidney Disease?
A renal diet for polycystic kidney disease (PKD) is based on GFR level and what stage of CKD you have. If you have PKD with normal kidney function (GFR >90ml/min), you have stage 1 CKD.
Please refer to the “What Is a Renal Diet for Chronic Kidney Disease?” above for more specific recommendations.
Sodium and fluid are especially important on a renal diet for people with PKD. Eating too much salt can cause faster cyst growth, in addition to raising blood pressure. (5)
A very high fluid intake is often recommended for people with PKD to slow cyst growth too! Drinking 3-4 liters of fluid each day reduces a hormone called “vasopressin”. Vasopressin can accelerate cyst growth in PKD. So, drinking a lot of water can help slow cyst growth. (5)
There are some new studies done in animals showing some promising benefits of a keto diet for PKD. However, more research is needed before this diet should be recommended to people with PKD. Learn more about the keto diet and PKD.
More about a healthy diet for polycystic kidney disease.
What Is a Renal Diet for People with a Kidney Transplant?
Nutrition is an important piece of protecting a new kidney! A renal diet after kidney transplant is individual to your lab values.
For most people, a renal diet after transplant is similar to the early stages of CKD. It is best to limit sodium and large amounts of protein, especially animal protein. Focusing on eating lots of fruits and vegetables will help keep your new kidney working as long as possible!
Food safety is also important for people with a transplant. Transplant medications impact your immune system and increase risk of foodborne illness. Learn how to keep your food safe!
What Is a Renal Diet for Proteinuria?
Proteinuria (or, too much protein in your urine) often goes hand-in-hand with kidney disease. Proteinuria is especially common for people who have kidney disease as a result of diabetes.
Kidney disease with proteinuria is usually more severe and progresses faster. So, we want to do everything we can to keep urine protein levels down!
Limiting protein (based on your stage of CKD) and sodium to 2,300mg/day will help lower protein in your urine. (1)
What Is a Renal Diet for Glomerulonephritis?
There are no special nutrition recommendations for glomerulonephritis. A renal diet for glomerulonephritis should be based on your GFR and stage of kidney disease.
What Is a Renal Diet for Kidney Stones?
There is no one renal diet that is good for kidney stones. Healthy eating for kidney stones is based on the type of stone you make and your 24-hour urine results. In my course, Kidney Stone Nutrition School, I teach you how to interpret your 24 hour urine results and tailor your diet for maximum stone prevention.
Calcium oxalate kidney stones are most common, and make up about 80% of kidney stones. The most common urine risk factor for kidney stones is hypercalciuria (or, high urine calcium). A dietary pattern that limits sodium to 2,300mg, non-dairy animal protein and added sugar can help lower urine calcium. (6)
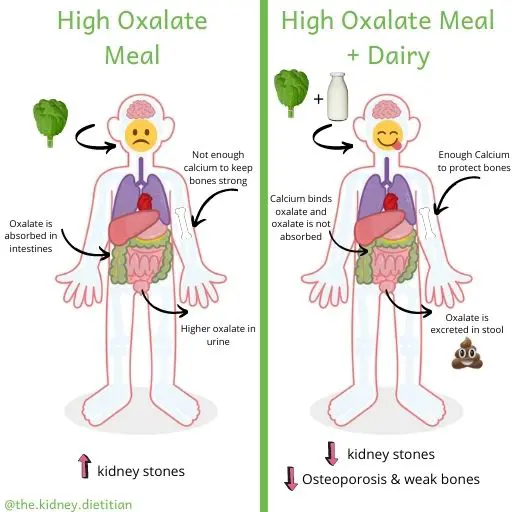
Contrary to popular belief, people who have calcium kidney stones actually need to make sure they eat enough calcium. (6)
No matter the type of kidney stone, drinking at least 3 liters of fluid each day is very important.
A low oxalate diet may also be important for kidney stone prevention. But, this is not the case for everyone.
Learn more about nutrition for calcium oxalate kidney stones. Or, read more about uric acid kidney stones.
Getting Help For a Renal Diet
As you can see, there really is NO one “renal diet”. A renal diet is individualized to your labs and medical history.
Putting all of this information together to figure out what to eat can be overwhelming. I highly recommend asking your nephrologist for a referral to meet with a Registered Dietitian to help you.
In the United States, most insurance covers dietitian visits for kidney disease! It is never too early (or, too late!) to work with a dietitian for kidney health.
For more help with kidney stones, check out my online course, Kidney Stone Nutrition School.
For more help with kidney disease, check out my resources page for a list of renal dietitians I love!
I also have a list of dietitians who specialize in kidney disease and have virtual practices on my resources page. The Academy of Nutrition & Dietetics and the National Kidney Foundation also have tools to help you find a renal dietitian near you!
Happy Eating!
Melanie

Hi,
Your information is very helpful and makes sense. I am stage 3 since 2020, and my doctor says I don’t need any renal dietitian at that stage. I want to believe that it would be helpful for me to have a meal plan scheduled.
I am a very concrete person and I don’t understand why is my doctor so resistant to refer me to a dietitian. Especially, when I experienced something weird recently.
My doctor can’t even explain that phenomenon.
I was treated with a wide range of antibiotics for a Diverticulitis, for a period of 6 weeks, on the IV fluids and no water or food intake.
Amazingly my Creatinine levels went down to below 1,
GFR went up to 79 and my leg swelling and
nocturia were gone completely during that treatment time. Right after that everything came back, and GFR is going down. What is the explanation for that, my doctor doesn’t know.
But my simple brain tells me, it’s either something in a diet or water I m eating and drinking that is ruining my kidneys. But my doctor says I don’t need a dietitian.
Or else, what’s in the IV fluid I am not receiving and I need?
I was a nice feeling to discover that my kidneys repaired or improved, I’d like to keep it that way.
I found it quite interesting, is there any scientific explanation for this phenomenon?
Also, wanted to share this.
Hi Margaret! I’m so glad my content has been helpful. It is ABSOLUTELY NOT too early to see a dietitian. Unfortunately, doctors often wait to refer people with CKD to dietitians until they are nearing dialysis or in the higher stages of CKD. We could make MUCH more difference in your health and kidney function is we meet with you as early as possible! I have a list of renal dietitians I recommend on my site if you want to take matters into your own hands!
please what kind of food should I give to my sister she has a kidney issues and it’s already at the stage 5 and she’s going for dailysis already,but my problem is that the doctor said if she can be going for dailysis 3 times a weak she can eat anything. so am not okay with that and am happy to see this site today please what’s best foods and fruit, soups that can be best for her please
Hello! Nutrition for kidney disease is different for every single person. I’d need to work with her and look at her labs to know what is best. I’d highly recommend working with a kidney dietitian to get all of your questions answered!
This was a very helpful article.
I am at stage 4 with a GFR of 29, I had been stage 3 & pre diabetic for a few years.
Really worried about the food I can eat.
I really liked what you said about diet & lab results, makes sense to me now.
Thank You for all your help.
Kathleen
I’m SO glad! Thank you for taking the time to leave a comment!
hello–I was just diagnosed 4 days ago with Stage 2 (no specific type) and told to drink more water and come back in 3 months. No info given on foods to avoid or increase. I also have chronic myelogenous leukemia since 9/2016, some mild heart issues and very bad burping and farting after a doctor stuck a tube down my throat for acid reflux. He told me it was a social issue and sloughed me off as tho I were a fly on his shoulder. I turned 79 in January and I am a never smoker since I tried one when I was 15 so I could be cool. I also have a bad attitude which is the only thing that has gotten me this far, well prayer is first then humor. Thank you so much for what you do and God bless you.
I have been being “seen” by a nephrologist for four years. He monitors my blood work. Got no other information or help from him. A chance remark by his PA told me I was in Stage 3, and that it’s “normal for your age.” I started reading online, and discovered that all along, I should have been in consultation with the nephrologist AND a renal dietician, and should have been on a dietary regimen of some kind. Now I am trying to connect dots, and found your site: it went ‘WAY farther than anything else I have found. THANK YOU for offering such a complete resource to people like me!!
Yay! I’m so glad my information is helpful to you. You are so welcome!!
Familiar Story Ralph: Finding the “right” information is a huge challenge.
Thank you for posting this very helpful article! You had some info that I couldn’t find anywhere else. I feel so much more confident that I’m doing the right things for my kidney health.
You are so welcome!! I’m glad it was helpful!
What are your thoughts on someone, 64 years old, with severe Acid reflux and resultant CKF stage 3a from PPis and well as genetically high cholesterol? 256 but weighing 110lbs.
Trying to maintain weight, cut out animal protein, manage acid reflux all at the same time is turning out to be a daunting task.
Thanks for any advice you may have.
Leslie
Hi Leslie! It is really important to balance getting adequate calories/nutrition with all of these renal diet restrictions that might be recommended for CKD or high cholesterol. For many people with CKD who need to gain weight, we focus on increasing healthy fats and carbohydrates to ensure adequate calorie intake. Without knowing more about you, I can’t safely provide specific advice for you. I’d highly recommend working with a renal dietitian to help you figure out the best balance for you!
Any diet recommendations for a person who will be having one kidney removed in a few weeks, due to an a small area of cancer cells that are described by the Dr. as “encapsulated”, with no evidence of cancer spread. There will not be radiation or chemo required. Both kidneys are normal functioning with e-GFR >60 and normal BUN and creatinine at recent lab draws. Does the remaining kidney work extra hard and are there modifications in protein, fluids, sodium, etc? Thank you.
Hi Joanne! I’m sorry to hear about your diagnosis, but happy it was caught! In general, people can eat a overall “normal” healthy diet with just 1 kidney. The kidneys are amazing and 1 really can do all the work that 2 of them can! More specific diet recommendations would be based on labs (like outlined in this article!), but usually there are not restrictions for potassium, fluid or protein. I’d probably just focus on staying healthy and preventing high blood pressure and diabetes to keep the 1 kidney going strong!
Thank you for this article it is so helpful for myself and my sister we both have CKD I’ve been trying to figure out what to eat to stay healthy! Thanks Debbie
Thank you so much for your kind message, Debbie! I’m so glad you found it useful!
Please send me a list of diet renal. Ineed to know what I can eat and foods I need to stay away from,I would like all the info I need. Thanks for it.
Hi Janice! A renal diet is all about learning how to build healthy eating patterns, and not just following a list of foods. Like this article talks about, there isn’t one “renal diet”. It is different for each patient based on your lab values and stage of CKD. I’d highly recommend asking for a dietitian consult to learn more about what is best for you!
Thank you for this information!!! I was diagnosed in December 2020 with stage 3 CKD! Got no info from Nephrologist on diet or anything else. Have been trying to learn on my own, but very confusing!! Got more info from your article today than any other source!! I am very visual so trying to copy info…wish I could get printed info!
Thank you so much Maxine! I’m SO happy you’ve found my site helpful. You could always print directly from my page. OR, I highly recommend The Cooking Doc’s book (on my resource page!) if you want much more reading similar to my stuff!
This was such a good article. I am thrilled to find you. I was diagnosed with CKD shortly before the pandemic hit. I attended a group “class” with a dietitian which was confusing. I have researched on my own and still find it difficult. I also need to lose weight so figuring out a diet that meets all my needs is exasperating. I did ask my primary for a referral to a RD but couldn’t get one til late July. This helps. Thank you
Hi Betsy! Thank you SO very much! Good for you for asking to meet with a renal RD. I know its far off, but, hopefully that gives you some more clarity. SO good to hear that this article helped as well!
i have a transplanted kidney, transplant took place on 01/12/2009. I was on dialysis from 2006 – 2009. The kidney is 13 now.
i am now at stage four CKD recent blood test kidney function 24. creatinine 157. I don’t want to go on dialysis again, its cruel.. i had a bad time with needles blowing, tubes bursting a lot of pain and cramp 3 times per wk. I kept my job on.. they were very accomodating. Im medically retired now and have the time to really look after myself. Apart from taking my meds and drinking lots of water, I would like to look at the best diet for me. I also have a pacemaker, Ive had it for about 8yrs now. I took a heart attack March 2022. I have other medical issues going on but not related to kidney. I would appreciate if you could lead me on the correct diet path for me to help my kidney function and creatinine
Thank you
Elizabeth
Hi Elizabeth! It sounds like you are very motivated to make changes for your kidney, heart and other health issues. This is amazing! I’d highly recommend working with a dietitian who can fully understand your medical history, labs and current eating habits and help you make changes. I have a list of kidney dietitians I recommend at my resources page. Best of luck to you!
This is such a valuable article. Thank you!
You are SO welcome! I’m glad you enjoyed it.
I can’t believe how many places I have looked for any food list to help me with my husband . He has diabetes and had a heart attack in Feb of 22. He is having kidney problems now with numbers in the 20’s. I can’t find a good food list for both diabetes and kidney. He is 75 and still works because he doesn’t want to (shrivel up and die) he says but he loves the bookwork. Thank you so much for the information you have printed here.
You are so welcome! This article might also be helpful!